|
|
Abstract
Thirty cases of post-acne scarring have been subjected to
treatment by low level energy diode laser (1450 nm) in 4-6
sessions at 3 week intervals. The duration of the study was 18 months
including a follow up period of 6 months after the last
session. Only 16 cases (53.3%) showed satisfactory (good to
excellent) response with a relatively high incidence of post
inflammatory hyperpigmentation (66.7%). Although low level
diode laser seems to offer an attractive modality to deal
with some dermal collagen disorders (as wrinkles and post
acne scars), the technique needs to be more refined and the
treatment regimens need to be more standardized so as to
achieve more consistent results, to optimize the response
and to minimize the incidence of side effects
Introduction
The use of lasers in dermal remodeling has started with
the so-called ablative lasers or laser resurfacing
especially with the use of CO2 laser and erbium YAG
laser.[1, 2, 3] However, the use of such lasers has been
associated with a relatively high degree of post operative
inconvenience as well as high rate of long term
complications especially prolonged redness, prolonged skin
intolerance to irritants in addition to high incidence of
dyschromias (whether hypo- or hyperpigmentation) [4, 5].
These complications besides the need of the patient to
interrupt his usual activities for relatively long periods
of time have paved the way for clinical trials on the use of
low levels of laser so as to achieve some sort of dermal
remodeling without, however, disrupting the surface
epidermis or in other words to make use of the
biostimulatory effect of low doses of laser rather than the
ablative effect of lasers when given in high doses.[5, 6]
The aim of the study was to assess the safety and efficacy
of one of these non-ablative lasers (low level energy 1450
nm-diode laser) in the treatment of a common problem that is
usually considered as a suitable indication for laser
resurfacing which is post acne scarring.
Patients and methods
Thirty cases of post acne
scarring of the face have been included in the study and
were subjected to treatment by low level energy 1450 nm
diode laser (Smoothbeam Candela Laser Corp., Wayland,
Massachusetts, USA). The patients have been collected at
random from The Dermatology Outpatient Clinic Bou Shahri
Medical Centre Kuwait, during the period from 3/2002 till
6/2002.
Excluded from the study were cases of numerous still active
acne lesions, those on concomitant treatment to the involved
skin area, patients who had received isotretinoin therapy in
the previous 12 months, cases with history of ablative
resurfacing procedures within 2 years of study initiation,
patients with keloidal tendency, pregnant females, patients
on photoactive or anticoagulant medications, those with
concomitant photosensitive dermatoses or connective tissue
disorders as well as those of Fitzpatrrick skin type V or VI
or having had recent sun tan in the previous 5 months.
In all subjects, areas of scarring on the face have been
subjected to 4-6 laser sessions at 3 week intervals using
low level energy 1450 nm diode laser (Smoothbeam-Candela)
with a spot size of 4 mm, at an energy fluence that varied
between 12 and 16 joules/square cm and using the standard
(built-in) triple pulse mode with a total pulse duration of
210 milliseconds. A special dynamic cooling device (DCD) has
been used for protective cooling of skin surface where there
are multiple bursts of cryogen spray (tetrafluoroethane,
_26 °C) in the form of 10 millisecond precooling, 10 - 15 ms
interpulse cooling and 10 - 20 ms posttreatment cooling (40
- 60 ms total). Chilling by DCD was adjusted to the level of
1 to 3 (corresponding to total burst duration of 40 to 60
milliseconds respectively). At each session, the areas
treated were subjected to a single pass of laser pulses with
no overlap. Beside the nature of the lesion and the skin
type of the patient, more precise dose adjustment was
carried out on the basis of a preliminary therapeutic test
in the preauricular region where the proper dose was that
causing mild to moderate erythema and oedema 10-20 minutes
after the test with no evidence of blistering or
unacceptable degree of discoloration at the initial 10 day
follow-up visit.
After each session, Patients were monitored for one hour to
determine any immediate side effects such as bruising,
blistering or intense erythema. They were advised to apply
some soothing cream (e.g. panthenol containing cream) till
disappearance of all signs of inflammation (usually for few
days). The patients were also asked to avoid exposure to any
type of physical or chemical irritation especially direct or
indirect sun throughout the period of study.
Initial and periodic clinical evaluation as well as digital
imaging were carried out at each treatment and follow up
visit (10 days after each session ) as well as 3 and 6 months
after the last session for the purpose of comparison and
objective evaluation of the result and side effects.
A modified scoring method has been used in this study to
describe the severity of the lesions in terms of number,
nature and depth of the scars as shown in table (1):
Table (1): Scoring method of the severity of the lesions in terms of number,
nature and depth of the scars
| Criterion |
Score
|
|
1 |
2 |
3 |
|
Nature |
saucer |
pitted |
punched out |
|
Depth |
shallow |
intermediate |
deep |
|
Size |
<2 mm |
2-5 mm |
> 5 mm |
The individual lesion score is defined
as the score of the lesion for depth multiplied by the
score of the same lesion for nature multiplied by its
score for size, while the total score for any particular case is
the sum of the individual scores of all the lesions in this patient.
Improvement was calculated as:
Patient's
total initial score - Patient's total score after treatment
|
% |
|
Patient's
total initial score
|
The degreeof improvement was defined as follows:
|
No
response
|
0% |
|
Weak response |
<15% |
|
Fair
response |
15-30% |
|
Good response |
30-50% |
|
Very good response |
50-75% |
|
Excellent response |
>75% |
Results
The study included 30 cases (11 males and
19 females) suffering from facial post acne scars . Their age rangied between 17 and 35 years (average 24.7). Ten
cases were of skin type II, 14 cases were of type III and 6
cases were of type IV.
The duration of the study was 18 months that include 6
months follow up following the last session. The total
number of sessions given was 169 and the average number per
case was 5.6 sessions. Table (2) shows group distribution of
patients according to the initial score, the number of cases
within each group and their percentage of the total number
of patients. Clinical evaluation of the follow up visits is
shown in Table (3) .
Table (2): Distribution of patients according to
the initial score
|
Initial score |
Number of patients |
Percentage |
|
< 30 |
2 |
6.7 % |
|
30 60 |
5 |
16.7 % |
|
60 90 |
5 |
16.7 % |
|
90 120 |
8 |
26.7 % |
|
120 150 |
7 |
23.3 % |
|
150 - 180 |
3 |
10 % |
Table (3): Clinical evaluation of follow up visits
following diode laser treatment of post acne scars.
Degree
Of Improvement |
Number of patients 10 days after session |
Number of patients |
|
1 |
2 |
3 |
4 |
5 |
6 |
3 months after last session |
6 months after last session |
| No response |
27
90% |
19
63.3% |
14
46.7% |
11
36.7% |
10
33.3% |
8
26.7% |
7
23.3% |
7
23.3% |
Weak
Response |
2
6.7% |
3
10% |
4
13.3% |
2
6.7% |
1
3.3% |
3
10% |
4
13.3% |
4
13.3% |
Fair
response |
1
3.3% |
7
23.3% |
7
23.3% |
11
36.7% |
8
26.7% |
7
23.3% |
3
10% |
3
10% |
Good
Response |
--- |
1
3.3% |
4
13.3% |
5
16.7% |
9
30% |
8
26.7% |
11
36.7% |
10
33.3% |
Very good
Response |
--- |
--- |
1
3.3% |
1
3.3% |
2
6.7% |
4
13.3% |
5
16.7% |
6
20% |
Excellent
response |
--- |
--- |
--- |
--- |
--- |
--- |
--- |
--- |
The overall evaluation 6 months after the last session
revealed no response in 7 cases (23.3% including 2 males and 5
females), weak response in 4 cases (13.3% including 2 males and 2
females), fair response in 3 cases (10% including 1 male and 2
females), good response in 10 cases (33.3% including 2 males and 8
females), very good response in 6 cases (20%) (4 males and 2
females) and no excellent response in any case (0 %),
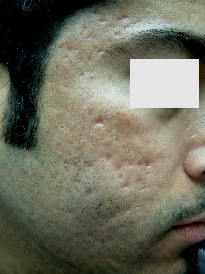
figures(1b, 1a, 2b, 2a, 3b, 3a,, 4b, 4a).
Improvement may become evident in exceptional cases - as
early as 10 days after the first session but usually not
before 10 days following the 2nd session. Atrophic
scars appeared to respond better than ice-pick scars. The
response is likely to continue with subsequent sessions
where cases showing any early (even weak) response were more
likely to show progressive improvement in subsequent
sessions than those with delayed response. Of interest is
that the improvement may continue for few months after
completely stopping the laser therapy especially in the
first 3 months following the last session. The
nature and incidence of side effects are shown in table (4)
Table (4):
The nature and incidence of side effects with low energy
diode laser treatment of post acne scars
| Nature |
No of patients |
Percentage |
Special remarks |
| Hyperpigmentation |
20 |
66.7 % |
-in darker skin
types
-with higher doses
-with higher cooling (>50 msec)
-usually mild, focal or incidental (not involving all the lesions treated) |
| Prolonged Redness (> one week) |
7 |
23.3 % |
| Blister formation |
6 |
20 % |
| Aggravation of scarring |
5 |
16.7 % |
| hypopigmentation |
3 |
10 % |
| ecchymosis |
2 |
6.7 % |
The most significant side effect was hyperpigmentation. The
latter tended to appear very early after the session (as
early as few hours after disappearance of the redness). It
was rather of the deep and ill-defined variety, usually of
low to moderate intensity, and showed tendency to extend for
few millimeters beyond the margin of the treated spot. It was more
with types III & IV skin especially with high energy doses
and/or high cooling settings. It tended to persist for several
months and was in general, slowly responsive to different
types of bleaching regimens.
 |
 |
|
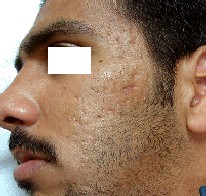
Fig. 1a: Before treatment. |
Fig. 1b: After treatment. |
 |
 |
|
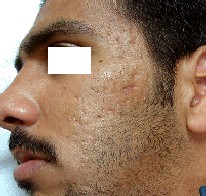
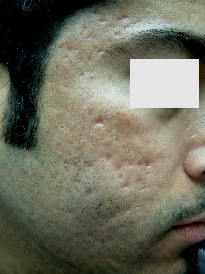
Fig. 2a: Before treatment. |
Fig. 2b: After treatment. |
 |
 |
| Fig. 3a: Before treatment. |
Fig. 3b: After treatment. |
 |
 |
| Fig. 4a: Before treatment. |
Fig. 4b: After treatment. |
Discussion
Apart from long term topical applications, currently
available methods for the improvement of skin texture
include dermabrasion, chemical peeling and laser resurfacing
(mainly with Erbium:YAG laser or CO2 laser). Among these,
ablative laser skin resurfacing was at a time considered the
mainstay for the so-called sculpturing of facial skin.[1,2,3].
At standard treatment parameters, these lasers ablate the
entire epidermis, part of the superficial dermis and impart
varying depths of coagulative tissue necrosis in the
residual tissue. Tissue ablation removes signs of
superficial photodamage and together with the residual
thermal damage initiates a normal healing response that
affects tissue tightening and prolonged stimulation of
neocollagen formation.[1,7, 8]
Although treatment with these systems consistently provides
significant improvement in photo-induced facial rhytides and
in atrophic scars, the typical 7-10 days during which re-epithelization
takes place result in prolonged postoperative recovery and
potentially troublesome adverse sequelae including prolonged
redness, oedema, milia formation.[1, 9] delayed healing,
postoperative pigmentary changes, infection and scarring[4].
For these reasons, research over the past few years has
focused on alternative modes of facial rejuvenation. Among
these, several (and optically different) non- ablative (or
low energy) lasers and light sources have been developed for
enhancement of scars and wrinkles without epidermal
disruption[5]. In these laser or light systems, heat is
generated within the zone of optimal penetration by direct
absorption of light energy. Heating decreases with increased
tissue depth as absorption and scattering attenuate the
incident beam The exact level of dermal damage in such non
ablative technique can be controlled by synchronization of
surface cooling and heating by laser (or light)[6]. The heated
dermis subsequently shows progressive changes in the dermal
collagen through the usual wound healing response where new
collagen formation and collagen remodeling occur in
association with removal of abnormal dermal collagen. The
thermal injury may also have a mechanical effect as it
results in disruption of collagen linkage with potential
collagen shrinkage and further collagen denaturation. In
addition to the wound healing and collagen shrinkage
effects, low grade inflammation induced by absorption of low
levels of laser light with subsequent release of
inflammatory mediators may result in further (but more
direct and probably more rapid) stimulation of fibroblastic
activity and new collagen formation [10].
Several types of laser have recently been available for such
purpose that markedly vary in the wave length of the laser
employed (and consequently the targeted chromophore and the
depth of penetration), the spot size, the pulse duration
(which -in general and with very few exceptions- is in the
order of few milliseconds) as well as the protective method
of surface cooling. One of these is the Smoothbeam laser
which is a low level energy diode laser (wave length 1450
nm). In this type of laser, the light is taken up by water
as its main absorbing chromophore. It has the theoretical
advantage of rather deep penetration into the skin due to
long wave length and poor absorption by other chromophores
thus ensuring delivery of a sufficient energy fluence with
subsequent thermal damage as low as 400 to 500 microns[6].
In earlier studies, non ablative lasers have been proved
safe and somewhat effective for improving wrinkles by
stimulating dermal collagen synthesis.[4,11] So, it seemed
rational that they might also be used to treat atrophic acne
scars.
The results of this study show that this newly emerging
laser modality can achieve some improvement in post acne
scarring. The improvement has been shown to progress (to a
variable degree) for several weeks to months after the laser
session probably indicating long-term stimulatory effect on
dermal fibroblasts besides the possible direct and more
rapid shrinkage, denaturation effects on dermal collagen and
elastic fibres[10].
The non-ablative ambulatory nature of the technique seems to
offer several advantages. There is no prolonged post
operative period in which the skin is scalded and during
which the patient has to rest at home. Furthermore, there is
no prolonged redness (in most cases) or skin
hyperirritability.
Using an optimal train of repeated pulses in Smoothbeam
laser device is far superior to a single pulse mode to
confine the thermal damage to the target tissue. The delay
between 2 consecutive pulses is properly adjusted so as to
give a chance for the epidermis to cool down and at the same
time maintain a steady state dermal temperature level where
the delay should be three to five times the thermal
relaxation time (TRT) of the target. Moreover, the depth of
the thermal injury could be
controlled by properly
selecting the number of pulses in the pulse train as well as
by properly adjusting energy fluence with surface cooling.
The protective effect for
the epidermis provided by the peculiar dynamic cooling
device (DCD) is another advantage of Smooth beam laser. A
previous study could show that cryogen spray cooling is
efficiently protective when used with non-ablative lasers as
it was with high energy lasers.[10] However,
preliminary test trials in the present study could clearly
show that critical adjustment of the cooling dose was
crucial as slightly higher than needed cooling was likely to
result in adverse effects more or less similar to high doses
of laser energy.
Moreover, the improvement
expected with the low level diode laser was found to be
rather inconsistent and to markedly vary from one patient to
another (depending upon not yet known factors). The response
was on average weak to moderate although some cases may show
unexpectedly impressive or rapid results. This variable
response may be explained at least in part- by interpatient
and site to site variability in the skin surface temperature
necessitating a range of optimal temperatures.
There is also the problem of
postinflammatory hyperpigmentation which occurred in few
cases of skin types II and many cases with skin types III &
IV. This hyperpigmentation was found to respond very slowly
to traditional bleaching treatments and might last for
several months after the procedure. Again this
hyperpigmentation was inconsistent and unpredictable being
variable not only from one patient to another but even from
one site to another in the same patient thus compromising
the predictive role of therapeutic tests.
It is not surprising that
non ablative laser systems can not achieve results
comparable to those of ablative lasers. Non ablative lasers
appear to be ideally suited for patients who are unable to
undergo an ablative laser procedure because of prolonged
recovery, for cases with only mild cutaneous pathology and
for those who would accept the tradeoff of a less dramatic
treatment benefit.
Conclusion
Although low level 1450 nm diode laser seems to offer an
attractive modality to deal with some dermal collagen
disorders (as wrinkles and post acne scars), both the
technology and the technique need to be more refined and the
treatment regimens need to be more standardized so as to
achieve more consistent results, to optimize the response
and to minimize the incidence of side effects.
References
1. Alster,T.S.(1999): Cutaneous resur-facing with co2 and erbium YAG lasers: preoperative, intraoperative and postoperative considerations. Plast. Reconstr. Surg. (103): 619-632.
2. Alster,T.S., Nanni, C.A.and Williams, C.M. (1999): Comparison of four carbon dioxide resurfacing lasers: a clinical and histopathological evaluation. Dermatol. Surg. (25): 153-159.
3. Alster,T.S. and Lupton, J.R.(2001): An overview of cutaneous laser resurfacing. Clin. Plast. Surg. (28): 37-52.
4. Goldberg, D.J. (2000): Full-face nonablative dermal remodeling with 1320 Nd:YAG laser. Dermtol.Surg. 26(10): 915.
5. Lupton, J.R., Williams, C.M. and Alster, T.S. (2002): Nonablative laser skin resurfacing using a 1450 nm Erbium glass laser: A clinical and histologic analysis. Dermatol. Surg. (28): 833 835.
6. Ross E.V., Sajben, F.P. and Hsia, J. (2000): Non ablative skin remodeling. Selective dermal heating with a mid-infrared laser and contact cooling combination. Lasers Surg Med (26): 186-195.
7. Ratner,D., Viron, A. and Puvion-Dutilleul, F. (1998): Pilot ultrastructural evaluation of human preauricular skin before and after high-energy pulsed carbon dioxide laser treatment. Arch. Dermatol. (134): 582-587.
8. Ross E., Naseef, G. and Skrobal, M.(1996): In-vivo dermal collagen shrinkage and remodeling following co2 laser resurfacing. Lasers Surg.Med.(18): 38.
9. Sriprachya-Anunt,S. , Fitzpatrick R.E. and Goldman M.P.(1997): Infections complicating pulsed carbon dioxide laser resurfacing for photoaged facial skin. Dermtol. Surg. (23): 527-536.
10. Silapunt S. and Goldberg, D.J. (2001): Optimal fluence and skin surface temperature in dermal remodeling with 1320 nm Nd:YAG laser. The Online Journal of Lasers and Cutaneous Cosmetic Surgery Issue: July.
11. Tanzi, E. L., Williams, C. M. and Alster T.S. (2003): Treatment of facil rhytides with a nonablative 1,450-nm diode laser: A controlled clinical and histologic study. Dermatol. Surg. 29(2): 124.
© 2004 Egyptian Dermatology Online Journal
|