|
|
Abstract:
The treatment of discoid lupus erythematosus with pulsed dye has been
evaluated in recent years. The improvement of telangiectasia and
erythema in cutaneous lesions was based on selective photothermolysis
ablation of the dilated capillaries and venules .While the improvement
in scar and atrophy was referred to the effect of pulsed dye laser on
collagenase activity. We describe the results of discoid lupus
erythematosus (DLE) lesions of 62 patients; they received treatment
with FPDL (585nm, 450µsec) with fluences ranged from 6.75 to
7.75J/cm².The overall clearance rate was 67.5%. Relapse had
occurred in 7 patients. Few side effects were observed in the form of
hyperpigmentation or hypopigmentation.
We confirm that pulsed dye laser is a good alternative treatment for discoid lupus erythematosus lesions.
Introduction
Classic discoid lupus erythematosus (DLE), the most common form of
chronic cutaneous LE, begins as flat or slightly elevated, well
demarcated red-purple macules, or papules with scaly surface. Early DLE
lesions most commonly evolve into larger coin-shaped (discoid)
erythematous plaques covered by prominent adherent scales. The lesions
slowly expand in association with active inflammation at the periphery,
leaving scarring with atrophy and telangiectasias at the center.
Chronic untreated cutaneous lupus erythematosus ends with marked
scarring; with depressed and contracted lesions on the face, creating a
wolf-like or lupus facieses [1].DLE skin lesions are present in 15-30% of variously selected study populations of SLE [2], [3].
The demonstration of immunoglobulin and complement proteins in the
dermal-epidermal junction of lesions from patients with DLE has led to
renewed interest in immunologic abnormalities of these patients [4].
Standard medical therapy includes corticosteroids (topical or
intralesional) and antimalarials. Other alternative therapies include
auranofin, thalidomide, oral or topical retinoids, and
immunosuppressive agents [5].
The flash lamp pulsed dye laser (585nm) was the first laser system
specifically developed for the treatment of cutaneous vascular lesions
such as port wine stains, telangiectasias and hemangiomas. It was based
on selective photothermolysis, which aims to destroy the blood vessels
of the cutaneous vascular lesions with minimal or no damage to the
surrounding tissue [6].
Patients and methods:
This study was conducted on 62 DLE patients who presented to our
dermatology laser outpatient clinic in the National Institute of
Laser Enhanced Science (NILES), referred from Al- Haud Al-Marsoud dermatology
hospital.
Patients of both sexes were included; 34 females, 28 males. Their age
ranged between 12 and 63 years, all skin types were included with no
prevalence to certain type. Follow up period was performed at 3,
6,12months after end of sessions.
Patients were diagnosed as classical type of DLE clinically,
pathologically and verified serologically. Both localized and diffuse
variants were included in the study.
Patients with signs and serological investigations suggestive of DLE
activity, females during pregnancy or postpartum were excluded from the
study.
Patients were divided into two groups according to distribution of the
lesions; localized DLE (48 patients) and disseminated DLE (14
patients).
-
Initial evaluation of patients to exclude the presence of SLE according to criteria stated by [7] was performed.
-
Pre and post treatment biopsies were taken.
-
Inter-rater reliability by two independent dermatologists at the
beginning of the treatment and at the end of laser sessions to assess
the degree of improvement.
-
Examination of the lesion to determine the following; site, size
extent, distribution and the present clinical signs of the lesions.
-
The signs of DLE were evaluated according to the severity as shown in table 1:
Table 1 .Evaluation of DLE signs
| |
None |
Mild |
Moderate |
Severe |
|
Erythema |
- |
+ |
++ |
+++ |
|
Telangiectasia |
- |
+ |
++ |
+++ |
|
Hyperkeratosis |
- |
+ |
++ |
+++ |
|
Atrophy |
- |
+ |
++ |
+++ |
-
The degree of improvement was determined as the percent reduction in
the clinical signs relative to normal surrounding skin in gradation of
10% to 100% rating.
-
Patients were photographically documented with digital camera; Kodak
DX 3700, 3.1 Mega pixels, 3 xs zoom before and after treatment. A
written consent to be photographed was taken.
-
Patients were evaluated every 2 sessions and at the end of treatment.
Laser procedure:
All the patients were treated by flash lamp pulsed dye laser; Candela
SPTL-1 (Candela Corp., Wayland, Mass.) with wave length 585nm, pulse
duration 450µsec and hand piece of spot size 5or 7mm.The energy
density employed ranged from 6.5 J/cm² to 7.5 J/cm² (average
7 J/ cm²), depending on the test treatment performed 8 weeks
previously.
Pathology procedure:
The histological sections were stained by hematoxylin & eosin,
and by a trichrome stain; then subjected to evaluation by an ordinary
light microscope. Epidermal thickness and blood vessels diameters were
measured with micrometry.
Results
The overall obtained clearance rate was 67.54% assessed by both subjective and objective means.
Itching is recorded by all patients to increase during the first week
after the laser session then gradually improved with subsidence of the
lesion at the end of treatment.
Regarding the signs; it was found that erythema improved first with
complete clearance of 74% followed by telangectasia which scored total
clearance of 57.1% at the end of sessions. The highest incidence of
complete clearance obtained was 85% which observed with hyperkeratosis;
however atrophy and scarring were the last signs to show improvement
with the least percentage of total clearance among clinical signs which
were 5.8% for atrophy and 5% for scar.
Tables from (1-5) show the distribution of patients according to
severity of each clinical sign and the number of patients that cleared
completely at the end of treatment.
It should be taken into consideration that not all the patients
presented the 5 clinical signs as the present clinical signs depend on
the stage of the disease i.e. old lesions presented with telangectasia
atrophy and depigmented scar while new lesions presented with erythema
,telangectasia, and hyperkeratosis only with no scar or atrophy.
Erythema:
At the beginning of treatment the total number of patients that had
erythema was 50 patients distributed according to severity as follows;
seven patients had mild erythema, while 30 patients were categorized as
moderate and 13 patients were of severe erythema. At the end of laser
sessions 34 patients were completely cured.
Although complete cure were not obtained in the other patients,
variable degree of improvement could be observed as shown in table 1.
Table 2 Distribution of patients according to the severity of erythema before treatment after treatment
Telangectasia:
Thirty-five patients had telangectasia with different degree of
severity while 15 patients were negative (telangectasia was not among
the presented clinical signs) before treatment
Table 3. The distribution of patients according to severity of telangiectasia before and after treatment.
 Figure (1) patient represents erythema and telangectasia before laser |

Figure (2) after laser
|
Hyperkeratosis:
Hyperkeratosis was presented as a clinical sign in 40 patients and its
improvement after treatment shows the highest clearance rate. The
distribution of the severity of hyperkeratosis was as shown in table 9
Table 4. The distribution of patients according to the severity of hyperkeratosis before and after treatment.
|

Figure (3) follicular hyperkeratosis
before laser |

Figure (4) after laser |
Atrophy:
Atrophy was presented in 26 patients, while 24 patients had no atrophy before treatment
Table 5. The distribution of patients before and after laser treatment according to severity of atrophy.
Scar:
Twenty-two patients had scar as one the presenting signs and 18
patients were scar free before treatment. Only one patient with mild
scar showed complete clearance. On the other hand the rest of patients
showed variable degree of improvement

Figure (5) atrophy and scar before laser |

Figure (6) after laser |
Table 6 . The distribution of scar patients according to the severity before and after treatment.
Effects of clinical variants on clearance of DLE lesions
Effect of size of the lesion, duration of illness, site of the lesion,
type of DLE and age were studied in relation to clearance rate.
Evaluation of the clearance rate at the end of laser sessions revealed that specific sites responded favorably than other sites.
Upon this observation the sites were divided according to its response
to treatment into responsive sites and less responsive sites
The less responsive sites were found on the scalp, lips and eye brow while the responsive sites include the rest of the body.
The clearance rate found to be higher in responsive sites than the less
responsive sites and this relation proved to be of highly statistical
significance p=0.004.
New lesions were found to respond better than old lesions and the former recorded higher clearance rate.
Regarding type of DLE; the mean of clearance rate of localized DLE
group was higher than that of disseminated DLE which proved to be of
high statistical significance p=0.010
Age of the patients was found to have a significant effect on the
clearance of the lesions. Patients younger than 35 years respond better
to treatment by laser and scored higher rate of clearance than those
who were older than 35 years which means that clearance rate decreased
with advance in age.
Among the previously outlined factors and their relations to the
clearance rate; it was found that age and duration of illness were the
only significant independent variables that affect the clearance rate
while the size of lesions was considered to be a dependent variable as
shown table 15
Table 6.Effect of multivariate on clearance rate
Patients were subjected for follow up period starting one month after the end of laser sessions then at 3, 6 and 12 months.
The data of follow up revealed that 42 patients committed the follow up
period on regular basis as they were instructed. Relapse occurred in 7
patients; one male and six females. Their ages ranged between 17-42
years. Four patients were of skin type III while the other three were
of skin type IV, V, and VI.
It is worthy to mention that 4 relapsed patients were on concomitant
systemic treatment; chloroquine during laser treatment and follow up
period. Results of effects of both clinical factors of the patients and
the characteristics of DLE lesions on occurrence of relapse could be
figured out as follows:
1. Both skin type and type of DLE have relation with relapse and this relations found to be of high statistical significance
2. Age, sex and site of lesions have minimal effects on relapse that of no statistical significance.
3. Concomitant treatment has no effect on relapse and this was proved statistically.
In this study 20 patients developed side effects; 17(85%) patients had
transient hyperpigmentation which fade after 3-6 months and 3 (15%)
patients had hypopigmentation.
Effect of pulsed dye laser on pathological characteristics of DLE:
Improvement of the pathological findings of DLE was confirmed by
recording the following changes in post laser biopsies which include;
decrease of hyperkeratosis and follicular horny plugging, marked
decrease of perivascular and periadenxal mononuclear inflammatory
infiltrates. Decrease of the dermal edema, blood vessels diameter and
epidermal thickness were recognized and confirmed by measuring before
and after laser treatment.
Improvement of the basal layer changes as loss of normal organization and vacuolation were much improved after laser treatment.
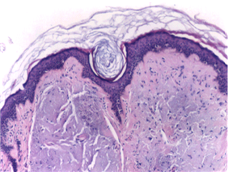
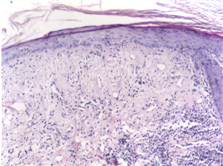
Figure (7) show the pathologic characteristics of DLE and Figure (8) show signs of improvement previously mentioned.
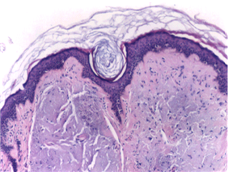
Figure (7) DLE histopathological changes
before laser |
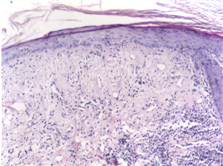
Figure (8) after laser
|
Discussion
Chronic discoid lupus erythematous (CDLE) is a skin disease
characterized by the presence of well-defined, raised erythematous
lesions that spread slowly with an irregular outline while the centers
of the lesions heal with scaling ,atrophy ,and scarring .Eventually
,the three events ;erythema ,hyperkeratosis and atrophy follow each
other .Active areas often show telangiectasia [8].
The flash lamp pulsed dye laser (FPDL) 585 nm with pulse duration
450µs was the first medical laser to develop specifically for the
treatment of vascular cutaneous disorders. It proved to be efficacious
and successfully used for the treatment of port wine stains,
hemangiomas and telangiectasias based on the principle of selective
photothermolysis, which aims to destroy the blood vessels of the
vascular lesions [9] because of its highly selective
targeting of the oxyhemoglobin molecule, thermal energy is released in
this very specific target within the vessel-the red blood cell. The
short pulse duration of this energy (450µs) spared the tissue
around from thermal damage [10], [11].
In 1986, Henderson and Odom [12] treated
characteristic plaques of DLE patient with carbon dioxide laser and
observed a dramatic clinical and cosmetic improvement of the cutaneous
lesion. Hypopigmentation in the tested areas and reactivation of DLE in
the periphery were described as side effect [12].
[13], [14] used argon laser in treatment of DLE, they documented successful trial. [15]
presented a case of lupus erythematosus telangiectoides in which the
main feature is telangiectasia, cutaneous atrophy was also present
.They used FPDL (585nm) at fluence of 7.25 -8.75 J/cm² in five
treatment sessions with 5mm spot size and a pulse duration 450µs(
SPTL-1 ,Candela). One year later [16] reported on 4
patients with telangiectatic chronic erythema of cutaneous lesions in
patients with systemic lupus erythematosus treated with the same laser
specifications and parameters; but the fluence used ranged from
6.75-7.75J/cm² in this study.
[17] Published on a group of 12 patients with
different forms of lupus erythematosus. In 10 patients, the lesions LE
was limited to the skin while two patients had systemic LE (SLE). They
were treated with the pulsed dye laser 585nm and an impulse duration of
0.3-0.45 ms (photo Genica V, Cynosure Inc,) they used handpiece with an
impulse diameter of 5mm, 7mm, and 10 mm. Depending on the spot size
used, the applied fluences were 3.4-3.5 J/cm² for 10mm handpiece,
3-7J/cm² for 7 mm handpiece, and 6-7 J/cm² for 5mm handpiece
,no anesthesia was used with their patients and they continue the
sessions until no further improvement was achieved the number of laser
sessions range from 1-10 in their study. In the most recent Egyptian
study done by [18], 4 patients of DLE were treated by
using PDL at either a wavelength of 585nm and short pulse duration and
fluence of 6-8.4 J/cm² for treating erythema mainly, and a
wavelength of 600 nm and long pulse duration and fluence of 3.8-7
J/cm² for treating telangiectasia at an interval of 4 weeks
between sessions.
All the available published studies focused on the effect of pulsed dye
laser as a tool for treatment of vascular lesions hence the improvement
of erythema and telangiectasia as they represent the vascular component
of DLE lesions neglecting its effects in treatment of other clinical
signs that contribute DLE lesions as hyperkeratosis, atrophy and
scarring
In this study 62 patients that were selectively chosen to be of
classical type of DLE without systemic involvement and this was
verified by serological investigation .Flashlamp pulsed dye laser 585nm
with pulse duration 450µs was used (SPTL-1, Candela). 5mm and 7mm
spot size were used for small and large size lesions respectively. The
energy density employed ranged from 6.5to 7.5 J/cm² (average 7 J/
cm²).
The present study included, all skin types except skin type I as it is
rare in Egyptians. Observations have raveled that patients with dark
skin type as IV-VI needed more laser sessions and this could be
explained by the proposal of [19] concerning melanin
absorption of visible light and its competition with oxyhemoglobin so
in patients with darker skin types more of the laser energy will be
absorbed within the pigmented epidermis ;this can result in
insufficient energy reaching blood vessels and increased incidence of
unwanted post inflammatory hyperpigmentation hence the need of more
sessions .
Based on the principle of selective photothermolysis proposed by [20]
and the vascular selectivity of the flashlamp pulsed dye laser (585nm)
cutaneous vascular lesions were treated successfully where the target
oxyhemoglobin in cutaneous blood vessels is selectively thermally
damaged that resulted in coagulative necrosis of red cells and
subsequent reduction in the number and size of cutaneous blood vessels.
FPDL proved its efficacy in treatment of port wine stains and
hemangiomas in children [21] and that explained the
effectiveness of FPDL in treatment of DLE as erythema and
telangiectasia are of the main clinical signs.
The microvascular damage may affect collagen or collagenase activity
within the scar .Thermal damage to abnormal collagen may allow
remodeling and reduction in endothelial cell volume that can affect
type V collagen. Mast cell alteration after laser irradiation may be of
importance. [22], [23].
On basis of the explanation proposed by previous authors, the
improvement of scars and atrophy of patients in this study could be
explained. [25], [26] ,[27].
[24] Treated 48 patients using fluences ranged from
6.5-7.5J/cm² and they have an 88% average improvement, with total
resolution in 20% after 4.4 treatment sessions. They found also that
facial scars less than one year old achieved better results than non
facial scars older than one year.
Comparing the results of complete clearance of scar in this study( 5%) to what has been obtained by [24]
could be referred to the chronicity of the scars ( more than one year)
as scarred tissue led to limited depth of penetration of the laser and
reduced number of blood vessels.
Explanation of improvement of hyperkeratosis and the pathological
changes of DLE is concerned with the role of dye laser in the
modulation of the inflammatory response of CLE. It has been observed
that the endothelial cell activation plays an important role in the
pathogenesis of lupus .This role could be due to the fact that higher
levels of adhesions molecules on the surface of the endothelial cells,
such as soluble E-selectin are correlated with active disease in LE
patients [28].
[29] Suggested that the selective destruction or
coagulation of the vessels leads to a modulation of the inflammatory
network and a regression of local lesions of DLE.
The activation of photosensitizing substance in the serum and
lymphocytes of LE patients could be demonstrated by irradiation at a
wavelength of 360-400nm [30], [31] while the action spectrum of LE does not include yellow light (585nm) dye laser [16].
It is well established that light energy in the ultraviolet (UV)
spectrum may precipitate or aggravate the disease in lupus
erythematosus [32].
[17] proposed that with laser therapy, the applied
light is monochromatic and there is strong evidence that the induced
pathogenic mechanism are different from those caused by irradiation
over a UV spectrum.
In the study done by [33], they stated that no induction of new lesions during treatment with FPDL.
Both age of patients and duration of illness have significant inverse
relationship with the clearance rate which mean that with younger
patients and short duration of illness the response to laser treatment
is much better than those of older age or with long duration of illness
that was expressed in the obtained higher clearance rate of the former
group.
Regarding the pathological process of DLE the three events; erythema,
hyperkeratosis and atrophy follow each other. Active areas often show
telangiectasia then healing occurred with scarring [34].
When atrophy and scarring occurred, the number of cutaneous blood
vessels is significantly reduced in the scarred tissue which is
targeted by this laser [17].
On basis of what had been mentioned, explanation of higher clearance
rate in new lesions that related to the short duration of illness
before the process of scarring had taken place.
An important observation has been found in this study on evaluation of
the clearance rate at the end of treatment in relation to the sites of
the DLE lesions. Specific sites responded favorably than others and
according to this observation the sites were divided into less
responsive sites, namely scalp, eyebrow and lips and responsive sites
in the rest of the body. Lower clearance rate was obtained with the
less responsive sites
Both scalp and eyebrow undergo irreversible scarring alopecia [1]
and as previously discussed the effect of scarring on the cutaneous
blood vessels therefore decreasing the response of the lesion to the
FPDL.
On the other hand the poor response of the lips could be referred to
the evaluation of response of port wine stain by dermatomal
distribution proposed by [35], [36].
It revealed that the upper cutaneous lip is V2 dermatome that responds
less favorably than V1 and V3 dermatome and they explained the
difference in response as V2 skin could be slightly thicker with more
adnexal structures and thus more vasculature and nerve endings. V2
dermatome includes the centrofacial part of the face (medial aspects of
cheeks, nose, and upper cutaneous lip).
However in this study complete clearance of DLE lesions in the cheeks
and nose was obtained so this postulation could not explain our result
clearly.
On discussing the effect of type of DLE on the clearance rate it is
worthy to mention that the clearance rate of localized DLE lesions was
much higher than that of disseminated DLE.
This may be explained by what [37] had found in their
study. On measuring the activity of the disease in both localized and
disseminated DLE; the former showed less activity hence the better
response to laser treatment.
Both studies that have done by [15], [16] found that no clinical deterioration seen at 16 weeks follow up of the reported case.
In the study done by [17] relapse was seen after 6
months after complete remission of the lesions in one case out of eight
patients that were subjected to follow up for 7 months .
Regarding the sex, results in this study matched with that of both [17], [33] where an observation has been made that all their relapsed cases were females.
This may explained by the effect of hormonal changes on the cutaneous disease in lupus erythematosus that studied by [38].They
observed premenstrual and perimenopause flare of the lesions and
improvement occurred after menopause. They also stated that the
replacement therapy has no effect on exacerbation of the disease. In
the present study two DDLE relapsed female patients developed SLE and
verified by serological investigations. The relapse in the rest of
female patients' could be referred to the effect of hormones
exacerbation of the disease and appearance of new lesions. The relapsed
male patient had been investigated serologically with no evidence of
disease activity but this patient was heavy smoker and smoking is
considered as one of the exacerbating factor as revealed by [39].
In the present study relapse has been found to occur more with disseminated DLE patients.
It could be suggested that the relapse is related to the activity of
the disease which leads to appearance of new lesions and according to
the study done by [37] to measure the activity of the
disease in patients with cutaneous lupus erythematosus by applying the
(SLAM); the Systemic Lupus Activity Measure proposed by rheumatologist
they found that L-DLE patients had less active disease than D-DLE.
Comparing the results of relapse in patients who continue on
concomitant treatment( systemic antimalarial) to those received no
medications during laser treatment, it was surprising to found that
relapse occurred more in those receiving systemic antimalarial. However
it is worthy to mention that with development of very active disease,
the antimalarials can not prevent such evolution [37].
The evidence of improvement of hyperkeratosis, horny plugs, edema and
marked decrease in the inflammatory cellular infiltrates was shown in
the post treatment biopsies compared to pre treatment one .The
organization of the basal cell layer and absence of the liquefactive
degeneration were another histological proof of clearance of DLE and
this was matched with
[33].
Measuring the blood vessels diameter before and after treatment has
revealed that marked reduction in both numbers and diameters of blood
vessels. These results were matched with what have been found by [16].
In this study measuring the epidermal thickness revealed that its
decrease by two folds in comparison to pretreatment measurement
Previous Histological investigations of FPDL tissue effects with
hematoxylin and eosin staining treatment in PWS patients have shown no [40] or minimal damage to the epidermis [41] at the light microscope level
By using the nitroblue-tetrazoliumchloride (NBTC) stain, that is a
histochemical stain NBTC stain demonstrate the epidermal damage after
FPDL treatment in most of their studied cases
To our knowledge this study will be the first in literature that proved
the occurrence of epidermal damage by measuring the epidermal thickness
at the light microscope level and coincide with what [42] reported on using NBTC stain. The presence of epidermal damage explains the clinical frequency of crust formation [11]
and the frequency of hyper -and hypopigmentation as the pigmented basal
cell layer is a primary target for the thermal damage. Hence, avoidance
of sun exposure seems essential before and during FPDL therapy [42].
By the aid of this valuable histopathological study done by the
previous authors many of the clinical findings in this study could be
explained as the hyperpigmentation, hypopigmentation presented with
dark skin type patients and their needs to more number of sessions to
achieve clinical improvement .This concur with the results of [43]
as they stated that the absorption of laser light in melanin leads to
thermal damage of the epidermis and subsequently , to lower dermal
energy fluences and less efficacy in vessel coagulation [44].In
this study the development of side effects were found to be presented
with the dark skin type and this concurs with that of [45],[43]; epidermal damage proved to be directly dependent on the intensity of epidermal pigmentation
Conclusions
Flash lamp pulsed dye laser were found to be an effective tool in
treatment of DLE lesions. Best results were obtained if used in
treatment of those fulfilling the following criteria; localized DLE
lesions that are confined to the responsive sites as was found in this
study that included the whole body except scalp, lips and eye brow. The
clearance rate obtained with young age patients less than 35 years and
short duration of illness was found to be associated with the best
results.
References
1. Sontheimer RD, Provost TT. Lupus
erythematosus. In: Sontheimer RD, Provost TT (eds). Cutaneous
Manifestations of Rheumatic diseases ed. Baltimore, Williams &
Wilkins 1997; PP 1-72.
2. Cervera R, Khamashta MA, Font J, et al. The
European Working Party on Systemic Lupus Erythematosus: Clinical and
immunologic patterns of disease expression in a cohort of 1,000
patients. Medicine 1993; 72:113.
3. Vlachoyiannopoulos PG ,Karassa FB, Karakostas
KX, et al. Systemic lupus erythematosus in Greece. Clinical features,
evolution and outcome, a descriptive analysis of 292 patients. Lupus
1993; 2:303.
4. Weigand DA. Cutaneous immunofluorescence. Med Clin North Am 1989; 73: 1263Lupus 1993; 2:303.
5. Callen JP. Treatment of cutaneous lesions in patients with lupus erythematosus. Dermatol Clin, 1994; 12:201-206.
6. Katugampola GA, Lanigan SW. Five years
experience of treating port wine stains with the flash lamp pulsed dye
laser.Br J Dermatol 1997; 137:750-754.
7. Fabbri P, Cardinali C, Giomi B, et al.
Cutaneous lupus erythematosus diagnosis and management. Am J Clin
Dermatol 2003; 4 (7).
8. Wallace DJ, Hahn BH. Dubois' lupus erythematosus. In Wallace DJ, Hahn BH (eds) 4th ed. Philadelphia: Lea & Febiger, 1993.
9. Tan OT, Murray S, Kuran SK. Action spectrum of
vascular specific injury using pulsed irradiation. J Invest Dermatol
1989; 92: 865-7
10. Esparza JR, Goldman MP, Fitzpatrick RE, et
al. Flash lamp pumped dye laser treatment of telangiectasia. Dermatol
Surg Oncol 1993; 1000-1003.
11. Garden JM, Bakus AD. Clinical efficacy of
the pulsed dye laser in the treatment of vascular lesions. J Dermatol
Surg Oncol 1993; 19: 321-326.
12. Henderson DL, Odom JC. Laser treatment of discoid lupus erythematosus. Lasers Surg Med 1986; 6: 12-5.
13. Zachariae H, Bjerring P, Gramers M. Argon
laser treatment of cutaneous vascular lesions in connective tissue
diseases. Acta Dermatol Venerol (Stockh) 1988; 68: 179-82.
14. Kuhn A, Becker-Wegerich PM, Ruzicka T, et
al. Successful treatment of Discoid lupus erythematosus with argon
laser. Dermatology 2000; 201: 175-177.
15. Nunez M, Boixeda P, Miralles ES. Pulsed dye
laser treatment in lupus erythematosus telangiectoides. Br J Dermatol
1995; 133:1010-11.
16. Nunez M, Boixeda P, Miralles ES. Pulsed dye
laser treatment of telangiectatic chronic erythema of cutaneous lupus
erythematosus. Arch Dermatol 1996; 132:354-59.
17. Raulin C, Schmidt C, Hellwig S. Cutaneous
lupus erythematosus. Treatment with pulsed dye laser.Br J Dermatol
1999; 141:1046-1050.
18. Saleh NF, Bosseila MAW, Zayed AA et al.
Pulsed dye laser treatment of erythema and telangiectasia in cases of
rosacea and discoid lupus erythematosus. Egypt J Derm& Androl.
Bound 2003; 23:21-28.
19. Tan OT, Kerschmann R, Parrish JA .The effect
of epidermal pigmentation on selective vascular effects of pulsed laser
.Lasers Surg Med 1984; 4:365-374.
20. Anderson RR, Parrish JA. Selective
photothermolysis: Precise microsurgery by selective absorption of
pulsed irradiation. Science 1983; 220: 524-527.
21. Tan OT, Morrison P, Kurban AK. 585 nm for the treatment of port wine stains. Plast Reconstr Surg 1990 (a); 86: 1112-1117.
22. Alster TS, Williams CM .Treatment of keloids
sternotomy scars with 585nm flashlamp-pumped dye laser. Lancet 1995;
345:1198-200.
23. Alster TS, McMeekin TO. Improvement of
facial acne scars by the 585 nm flashlamp -pumped pulsed dye laser. J
Am Acad Dermatol 1996; 35:79-81.
24. Goldman MP, Fitzpatrick RE. Laser treatment of scars. Dermatol Surg 1995; 21:685-687.
25. McDaniel DH, Ash K, Zukowski M .Treatment of
stretch marks with the 585 nm flashlamp -pumped pulsed dye laser.
Dermatol Surg 1996; 22:332-337.
26. Alster TS. Laser treatment of hypertrophic scars, keloids and striae.Dermatol Clin 1997(a); 15:419-429.
27. Narurkar V, Haas A .The efficacy of the 585
nm flashlamp pulsed dye laser on striae distensae at various locations
and etiologic factors ,lasers Surg Med Suppl 1997; 9: 35.
28. Orteu CH, Sontheimer RD, Dutz JP. The
pathophysiology of photosensitivity in lupus erythematosus.
Photodermatol photoimmuonol photomed 2001; 17:95-113.
29. Nürnberg W, Algermissen B, Hermes B, et
al. Erfolgreiche Behandlung des chronisch diskoiden lupus erythematodes
mittels Argon -laser. Hautarzi 1996; 47:767-770(translated).
30. Lehmann P, Holzle E, Kind P, et
al.Experimental reproduction of skin lesions in lupus erythematosus by
UVA and UVB radiation Am Acad Dermatol 1990; 24:376-378.
31. Kind P, Lehmann P, Plewig G. Phototesting in lupus erythematosus .J Invest Dermatol 1993; 100(Suppl):53-57.
32. Bennion SD, Norris DA. Ultraviolet light
modulation of auto antigens, epidermal cytokines and adhesion molecules
as contributing factors of the pathogenesis of cutaneous LE. Lupus
1997; 6: 181-192.
33. Baniandrés O, Boixeda P, Belmar P, et
al. Treatment of lupus erythematosus with pulsed dye laser. Lasers in
Surg and med 2003; 32:327-330.
34. Rothfield NF. Cutaneous manifestations of
multisystem diseases. In: Fitzpatrick TB, Freeberg IM, Eisen AZ, Wolff
K, Austen KF, Goldsmith LA, Katz SI, eds. In:Dermatology in general
medicine. 4th ed.vol 2.Library of Congress1995; pp2130.
35. Renfro L, Geronemus RG. Anatomical
differences of port wine stain in response to treatment with pulsed dye
laser .Arch Dermatol 1993; 129:182-8.
36. Orten SS, Waner WL, Flock S et al. Port wine
stains: an assessment of 5 years of treatment. Arch Otolaryngol Head
Neck Surg 1996; 122:1174.
37. Parodi A, Massone C, Cacciapuoti M, et al.
Measuring the activity of the disease in patients with cutaneous lupus
erythematosus . Br J Dermatol 2000; 142:475-460.
38. Yell JA, Burge SM .The effect of hormonal
changes on cutaneous disease in lupus erythematosus. Br J Dermatol
1993; 129:18-22.
39. Rook A, Wilkinson DS, Ebling FJ. Lupus
erythematosus in: Textbook of dermatology .Champion RH, Puton JL. Burns
DA, Breathanch SM, eds. 6th edn, Vol. 3 Oxford: Blackwell Science,
1998; 2488 - 501.
40. Tan OT, Carney M, Margolis R, et al.
Histologic responses of port wine stains treated by argon, carbon
dioxide, and tunable dye lasers. Arch Dermatol 1986; 122:1016-1022.
41. Tan OT ,Stafforod TJ, Murray S et al
.Histologic comparison of the pulsed dye laser and copper vapor laser
effects on pig skin .Laser Surg Med 1990 (b);10:551-558.
42. Hohenleutner, Hilbert M ,Wlotzke U et al.
Epidermal damage and limited coagulation depth with flash lamp pulsed
dye laser : A histochemical study .J Invest Dermatol 1995;104:798-802.
43. Tong AKF ,Tan OT, Boll J ,et al.
Ultrastructure effect of melanin pigment on target specificity using a
pulsed dye laser (575) .J Invest Dermatol 1987; 88:747-752.
44. Goldman MP, Fitzpatrick RE. Treatment of
cutaneous vascular lesions In: Goldman MP and Fitzpatrick RE (eds).
Cutaneous laser surgery. Mosby, St. Louis, 2nd edition. 1999; PP 19-178.
45. Garden JM, Tan OT, Kerschmann K, et al.
Effect of dye laser pulse duration on selective cutaneous vascular
injury. J Invest Dermatol 1986; 87: 653-657.
© 2006 Egyptian Dermatology
Online Journal
|