Abstract:
Objectives:
To compare between pulsed dye laser and podophyllin resin in treatment
of genital warts regarding pain, number of sessions, clearance rate, and
recurrence.
Methods:
Thirty-nine female patients were divided into two groups, the first group;
20 patients was treated with podophyllin resin, the second group 19 patients
was treated with pulsed dye laser (Candela) 595nm, 1.5 ms pulse duration,
7mm spot size and fluence 12-15 J/cm²
Results:
Complete cure rate was observed in both groups, but recurrence occured
in only 5 patients treated with podophyllin resin during follow up period.
Conclusion:
Both treatments are effective equally regarding the clearance rate but
FPDL is superior to podophyllin resin concerning the recurrence.
Introduction:
The prevalence of genital warts is increasing globally, and is estimated
to be about 1% in the sexually active population [1].
It has been estimated that at least half of all sexually active individuals
will acquire Human Papilloma Virus (HPV) at some point in their lives, whereas
at least 80% of women will acquire an HPV infection by the age of 50 [2].
The HPV viruses are known to invade the squamous epithelium of the entire
lower female genital tract, [3]. They usually
appear after a latency period of six months or more. The main risk factors
for contracting the virus include early beginning of sexual life and multiple
sexual partners. Congenital or acquired immunodeficiencies also favor the
appearance and persistence of the warts .Vulval HPV warts can cause significant
physical discomfort, including inflammation, itching, bleeding and dyspareunia.
Although HPV warts are usually benign growth, certain types of HPV pose
a potential risk of developing cancer [4].
Many modalities have been used to treat HPV-associated warts such as
5-fluorouracil and interferon that are not recommended because of their
low efficacy and toxicity. Trichloroacetic acid is a widely used non-surgical
therapy, but little is known about its efficacy, and is associated with
unpleasant side-effects. Imiquimod and podophyllotoxin are recommended in
both Europe and the US. The wart clearance rates for these two treatments
are similar, although imiquimod is associated with lower recurrence rates
and is more expensive [5].
Studies suggest that surgical therapies, including cryotherapy, electrotherapy,
and surgical excision are largely equivalent to one another with respect
to clearance rates Moreover; these may require anesthesia and have been
painful, leading to discomfort among patients. Another major concern, especially
with the use of high density CO2, is the risk it may have, to the patient
and staff, from HPV DNA contamination during the procedure [6].
Podophyllin is a crude extract prepared from the roots of different species
of Berberiacae (May apple). It is not a uniform substance and contains a
number of active constituents. It has the advantage of being a cost-effective
treatment and, accordingly it has been recommended as an appropriate first-line
agent. [7]
The Flash lamp Pulsed Dye Laser (FPDL) 595 nm with pulse duration 1.5ms
proved to be efficacious and was reported to be successfully used for the
treatment of many skin lesions including port wine stains, hemangiomas ,
telangiectasias and genital warts. This efficacy is based on the principle
of selective photothermolysis, which aims to destroy the blood vessels of
the vascular lesions. It is the highly selective targeting of the oxyhemoglobin
molecule, which absorbs the thermal energy of this wavelength, which is
released in this very specific target within the vessel - the red blood
cell. The pulse duration of this energy (1.5ms) spares the tissue around
from thermal damage [8].
This study adopts to explore further the use of pulsed dye laser and
evaluate its impact on vulval HPV treatment in comparison with podophyllin
resin regarding four important issues: 1) number of sessions till complete
clearance obtained 2) pain associated with treatment, 3) rate of clearance
of warts and 4) recurrence of the lesions.
Patients and methods:
Within 12 months, this study was conducted on 39 female patients with
external genital warts in the outpatient dermatology clinic, National Institute
of Laser Enhanced Sciences Cairo University, Egypt.
Patients were voluntarily included in the study after providing informed
consent. Pregnant females and patients who previously had treatment for
their warts were excluded from the study.
Inclusions criteria in this study were warts count up to 15 and diameter
below 10 cm. The genital warts were divided according to the site into;
vulval, anal and anogenital (figure 1). Patients were divided into two randomized
groups. The first group (group I) included 20 patients who were treated
with podophyllin resin solution 20% dissolved in alcohol that was applied
to warts. Areas adjacent to warts were protected and covered by a Vaseline
layer. Weekly Sessions were repeated until complete recovery was obtained.
The second group included 19 patients treated with flashlamp pulsed dye
laser (FPDL) 595nm (Candela) with a Dynamic Cooling Device (DCD) cryogen
spray time 30 ms, delay time 10 ms, pulse duration 1.5 ms, fluence 12-15
J/cm², 7mm spot size and 3-4 sequential pulses were applied till grayish
white color of the wart was obtained. Sessions were performed every 2 weeks.
We based the joules settings on the standard settings in literature and
the subjective opinion of the physician with regard to the size and thickness
of the wart. Fucicortâ cream (Fusidic acid 2%+Betamethasone 0.1% preserved
with chlorocresol ) manufactured by LEO pharma. Inc. was advised to patients
for one week following session.
Pain scoring was measured in two ways: 1) through the use of the visual
pain analogue score where the patient gave a score of 0 to 10, where 0 indicates
no pain, and 10 indicates excruciating pain; 2) through assessing patients’
perception about the pain. During the procedure, patients were asked to
indicate whether they perceived the pain as painful or sever pain, hot or
moderate pain, warm or mild pain, and no pain.
Each patient was followed up for six months. Visible clearance of warts
was assessed using naked eye inspection at 1, 3 and 6 months after the initial
treatment.
Statistical methods:
· Data were collected on special format, verified and then coded when
needed prior to analysis.
· All continuous data were expressed as mean±SD; categorical data were
expressed as frequency in tables.
· For comparative purposed between groups, in all continuous data independent
t-test ANOVA test were performed.
· Chi- square test for testing association in categorical data.
· Value 0.05 was considered significant as Confidence interval 95% was
set.
· Analysis has been performed using SPSS12 and graphics by Excel.
Results:
The mean age of patients was 35. 9±13.3 years (range 25 to 60)
All patients of both groups show complete remission after an average
of
2.6±1.1 sessions, (range 1-4) for Group I and 2.9±1.4 sessions (range
1-5) for group II.
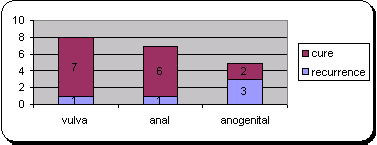
 | Fig 1:
Shows distribution of number of patients of each group in
relation to site of genital warts. |
|
1. Number of sessions:
We found that patients with vulval warts needed less number of sessions
to have complete cure compared to anal and anogenital types for both groups
(table 1, 2).This was statistically significant p=0.0001 for group I and
p=0.05 for group II
|
Site |
N |
Mean of sessions± Std.dev |
P value |
|
Vulva |
11 |
1.8±0.6 |
0.0001 |
|
Anal |
5 |
4.4±0.5 |
|
Anogenital |
3 |
4.6±0.5 |
Table (1): Relation between number of sessions and site of warts in laser
treatment group
|
Site |
N |
Mean of sessions ± Std.dev |
P value |
|
Vulva |
8 |
1.3±0.5 |
0.05 |
|
Anal |
7 |
3.1±0.3 |
|
Anogenital |
5 |
3.8±0.4 |
*N= number of patients
Table (2): Relation between number of sessions and site of warts in podophyllin
treatment group
 | Fig
2: Relationship between number of sessions and site of
lesions concerning both groups. |
|
2. Pain:
Assessment of patients’ rating of the pain showed that 80% experienced
minimal discomfort and were pleased to complete the procedure. The mean
visual pain analogue scoring was 4.6 and 2.05 for podophyllin and laser
groups respectively, with a range from 1 to 8 and 1 to 7 for podophyllin
and laser groups respectively (Table3). It is worthy to mention that ulceration
and edema were reported by 2 patients that treated with podophyllin resin
in the first 2 days following the session.
| |
Pain score
(0 – 10) |
Mean pain score |
| |
1 - 3 |
4 - 7 |
8 - 10 |
0 - 10 |
| Group I |
n=9 |
n=5 |
n=6 |
4.6 |
| Group II |
n=16 |
n=3 |
n=0 |
2.05 |
*N=number of patients
Table (3): Visual Pain Analogue Score by Site of Lesion during and immediately
after the first session of treatment.
3. Recurrence:
Recurrence occurred in 5(25%) patients of group I treated with podophyllin
during follow up. The anogenital site was observed to have the highest recurrence
yet it didn’t match statistical significance level
|
site |
vulva |
anal |
anogenital |
P value |
|
Recurrence |
1 |
1 |
3 |
0.448 |
|
|
|
|
|
20% |
20% |
60% |
|
Complete cure |
7 |
6 |
2 |
|
|
|
|
|
46.70% |
40% |
13.30% |
Table (4): Relation between clearance rate and site in podophyllin treated
group I
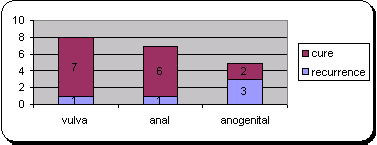 | Fig
3: shows relation between recurrence and site of lesion in
podophyllin treated group I |
|
Discussion:
Genital warts represent benign epithelial proliferations induced by human
papilloma virus (HPV). Many lines of treatment exist, but the results are
not satisfactory because of the high relapse rate (10).
Badawi et al., 2006 found complete resolution of treated warts achieved
in 96% of lesions as 174 male patients were treated by using pulsed dye
laser (wavelength 585nm, 0.45ms pulse duration Cynosure) with5- 7mm spot
size; fluence 9-10J/cm, recurrence rate was 5%(11). Komericki et al., 2006
treated 22 patients with FPDL that all patients in the study had complete
resolution after 1-5 laser sessions with no complication or scarring (12).
In study done by Tuncel et al., 2002 both 585nm and 595nm FPDL were used
with equal results of success and they claimed achieving complete cure after
one session (13). We used FPDL with wavelength 595nm, 1.5 ms pulse duration,
fluence 12-15 J/cm². The long wavelength offered longer depth of penetration
(14). DCD cryogen (spray time 30, delay time 10) reduced pain markedly during
sessions.
The mechanism of action of FPDL is not fully understood. One histological
feature of wart is dilated and congested blood vessels in the dermal papillae.
This blood vessel may be responsible for the viability of the wart.T The
pulsed dye laser destroys vessels by selective photothermolysis of oxyhemoglobin
(15). In addition HPV is heat sensitive and lasers may destroy the virus
by thermal effect (16). The principle action of Podophyllin is through binding
to microtubules sub-units and arresting cell division mitosis. Podophyllin
may cause local adverse effects such as inflammation, edema, and ulceration.
Teratogenicity and intrauterine fetal death had been described (17). Severe
systemic toxicity may arise after topical use of podophyllin, most commonly
when used in large volumes (17, 18).
On studying the possible relation between site of warts and number of
sessions needed we found that the anogenital warts disappearance "regardless
their number" needed more sessions in both types of treatment compared to
vulval and anal warts. The difference was statistically significant p=0.0001
for group I and p=0.05 for group II. (table 1, 2).
It was also found that recurrence of the 5 patients treated with podophyllin
occurred in 3 patients with anogenital warts.
Conclusions:
Both treatments are effective equally regarding the clearance rate but
FPDL is superior to podophyllin resin concerning the rate of recurrence
and post session pain, edema, and ulceration.
References
1. Koutsky LA, Kiviat NB. Genital human papillomavirus.
In: Holmes KK, Sparling PF, Mardh PA, Lemon SM, Stamm WE, Piot P, et al.,
editors. Sexually transmitted diseases. 3rd ed. Vol.1. New York: McGraw-Hill
Health Profession Division; 1999.p. 347-59.
2. Maw RD, Reitano M, Roy M. An international survey of
patients with genital warts; perceptions regarding treatment and impact
on lifestyle. Int J STD AIDS; 9:571-8 (1998).
3. Ferenczy A, Mitao M, Nagai N, Silverstein SJ et al. Latent
papillomavirus and recurring genital warts. N Engl J Med 313: 784–788 (1985).
4. Shamanin V, Glover M, Rausch C et al. Specific types
of human papillomavirus founded in benign proliferations and carcinomas
of the skin in immunosuppressed patients. Cancer Res.P.229-77 (1994).
5. Beutner, KR, Ferenczy A: Therapeutic approaches to genital
warts. Am J Med 102: 28–37 (1997).
6. Lacey CJ. Therapy for human papillomavirus-related disease.
J Clin Virol 2005;32 (Suppl. 1):S82-S90 .
7. Claesson U, Lassus A, Happonen H et al. Topical treatment
of venereal warts: a comparative open study of podophyllotoxin cream versus
solution. Int J STD AIDS; 7:429-34 (1996).
8. Katugampola GA, Lanigan SW. Five years experience of
treating port wine stains with the flash lamp pulsed dye laser.Br J Dermatol;
137:750-754. (1997).
9. Ferenczy A.: Laser treatment of genital human papillomavirus
infections in the male patient. Obst Gyn Clin N Am18: 525–535 (1991).
10. Schneede M ,Meyer T, Ziller P. Clinical and Viral Clearance
of Human Papillomavirus(HPV)-Associated Genital Lesions by Nd:YAG-Laser
Treatment Med. Laser Appl. 16: 38–42 (2001).
11. Badawi A, Shokeir HA, Salem AM et al. Treatment of
genital wart in males by pulsed dye laser J Cosmet Laser Ther.8(2):92-5
(2006).
12. Komericki P, Akkilic M, Kopera D. Pulsed dye laser
treatment of genital warts. Lasers Surg Med., 38(4):273-6(2006).
13. Tuncel A, Gorgu M, Ayhan M et al. Treatment of anogenital
wart by pulsed dye laser .Dermatol Surg.28(4):350-2 (2002).
14. Anderson RR, Parrish JA. Selective photothermolysis:
Precise microsurgery by selective absorption of pulsed irradiation. Science;
220: 524-527(1983).
15. Kenton-Smith J, Tan s. Pulsed dye laser therapy for
viral wart.Br J Plast Sur, 52:554-8(1999).
16. Vargas H, Hove C, Dupree m et al. The treatment of
facial verrucea with pulsed dye laser. The laryngngoscope, 112:1573-6(2002).
17. Fraser PA, Lacey CJN, Maw RD. Motion: podophyllotoxin
is superior to podophyllin in the treatment of genital warts . J Eur Acad
Dermatol Venereol; 2:328-34 (1993).
18. Robson K, Cunningham N, Kruzan K et al. Pulsed dye
laser versus conventional therapy in the treatment of warts: a prospective
randomized trial. J Am Dermatol, 43:275-80(2002).
© 2007 Egyptian Dermatology Online Journal
|