|
|
Abstract:
Objective To determine the psychiatric morbidity and quality of life (QOL) in three common dermatologic disorders namely vitiligo, psoriasis and alopecia areata (AA) in Egyptian patients attending Dermatology Outpatient Clinic, Ain Shams University hospital.
Patients and Methods: The study included 150 patients (3 groups; each of 50 patients with psoriasis, vitiligo and AA). The patients in this study were subjected to QOL assessment by 2 questionnaires [PCASEE and dermatology life quality index(DLQI)] and psychiatric evaluation using general health questionnaire (GHQ). For evaluating psychological distress, we used Taylor manifest anxiety scale for anxiety assessment and Zung scale for depression assessment.
Results: Psychiatric morbidity was detected in 34% of vitiligo patients, 38% of psoriasis patients and 36% of AA patients. Anxiety was detected in 14% of vitiligo patients, 12% of psoriasis patients and 24% of AA patients. Depression was detected in 24% of vitiligo patients, 30% of psoriasis patients and 16% of AA patients. Disease severity was significantly higher in psychiatric morbidity positive cases in the 3 studied groups (P<0.05). Suicidal thoughts were significantly related to the disease severity in the 3 studied groups (P<0.05). In psoriasis patients only, pruritic symptoms were detected in significantly larger number of patients with psychiatric morbidity (15 of total 19) than in those without psychiatric morbidity (10 of 31) (P<0.05). The mean score of QOL was significantly worse in psychiatric morbidity positive patients than psychiatric morbidity negative patients. Psoriasis had the worst QOL compared to the other 2 studied groups. There was a highly significant relation between poorer QOL and depression and anxiety in the 3 disease groups by both DLQI and PCASEE.
Conclusions: Vitiligo, psoriasis and AA are commonly associated with psychiatric morbidity. We found a strong association between psychiatric morbidity and poorer QOL in the 3 disease groups. It is important for dermatologists to understand the profound effect of these diseases on the QOL and to know the psychosocial and psychiatric consequences of these diseases. We should evaluate the effect of the different types of treatment or psychological intervention on improving the QOL of the patients and on the course of these diseases. Introduction:
Skin is the most visible organ which determines to a great extent our appearance and plays a major function in social communication and sexual attractiveness [1]. Thus, the skin condition may have a considerable impact on the patient's well being. The relationship between psychological factors and dermatological diseases has long been noticed e.g. stress can precipitate or exacerbate a skin disease through psychosomatic mechanisms [2]. Significant psychiatric and psychological morbidity is present in at least 30% of dermatological patients. Diseases involved in such context include acne, psoriasis, vitiligo, atopic dermatitis, urticaria and angioedema. They are all commonly seen in primary care. Consideration of psychological factors and recognition of patients who may be at high risk of developing such comorbidity are thus essential for effective management of these skin disorders [3,4,5]. Regardless of psychiatric morbidity, skin diseases can greatly affect patient's quality of life (QOL). Thus, patient oriented QOL measures are particularly beneficial in chronic diseases as they assess how the diseases affect a person socially, psychologically and physically [6]. The aim of this study is to determine the psychiatric morbidity and QOL in three common dermatologic conditions which are vitiligo, psoriasis and alopecia areata (AA) in Egyptian patients attending the Dermatology Outpatient Clinic, Ain Shams University hospital. Patients and Methods:
This study included 150 patients (3 groups; each of 50 patients with psoriasis, vitiligo and AA). All patients were recruited from the dermatology outpatient clinic, Ain Shams University hospital between June and December, 2006. Patients' age ranged from 18 - 65 years. The disease duration ranged from 1-26 years. We excluded patients with chronic debilitating diseases as cancer, liver, renal and cardiac diseases, hypertension, diabetes, pregnant or lactating women and patients receiving psychotropic drugs. All subjects of the study gave their informed consent prior to participation in this study and were subjected to the following:
|
(A) |
Full history taking including exacerbating factors. |
| (B) |
Thorough general and dermatological examination. |
| (C) |
Severity scoring: by:
|
| -
|
Psoriasis area and severity index (PASI) score for psoriasis patients [7]. |
| - |
Severity of alopecia
tool (SALT) score for alopecia areata patients , the scoring
was done as follows : |
| |
S: scalp hair
loss ( S0= No hair loss , S1=
≤
25% hair loss , S2 = 26- 50% hair loss, S3= 51- 75% hair loss, S4=
76- 99% hair loss, and S5= 100% hair loss ); B: body hair loss ( B0=
no body hair loss , B1= some body hair loss , and B2=100% body hair
loss ) [8]. |
| -
|
Body percentage of surface area (BSA) involved according to the rule of nines for vitiligo patients [9]. |
| (D) |
QOL and psychiatric evaluation: |
|
- |
QOL: it was evaluated by 2
questionnaires: |
| - |
PCASEE[10]:
This includes life quality questions which measure the following
parameters: |
| |
- P (physical
problems).
- C (cognitive problems).
- A (affective problems).
- S (social problems).
- E (economic problems).
- E (ego problems). |
| The Arabic
version by Sadek et al. (2003) [11]
was used in this study. Higher scores of total PCASEE indicate a
better QOL. |
| - |
The dermatology life quality index (DLQI) [12]: It consists of 10 questions with simple tick box answers scored from zero to three. It is designed for use in adults i.e. patients over 16 years old. It is calculated by summing the scores of each question. The higher the score, the more the QOL is impaired. |
| - |
Psychiatric evaluation: |
| 1- |
General health
questionnaire (GHQ) [13]: It was used to evaluate psychological distress in all patients. It is a self report scale which provides an indication of psychological distress. It consists of 28 items and was used in its Arabic version [14]. Scores are given on a 2 point linear scale (0 for better than usual or usual and 1 for less than usual or very less than usual). Higher scores indicate a higher level of psychological distress and those scored above cut off points (7 or more) were subjected to assessment for depression and anxiety. |
| 2- |
Taylor manifest
anxiety scale [15]: translated and validated in Arabic by Fahmi et al. (1977) [16]. It assesses the subject's awareness of estimate and willingness to report emotional habitual response rather than feeling at the time of completion of the scale. It consists of 50 items.
Interpretation: zero-16: normal, 17-24: mild, 25-35: moderate, 36-50: severe. |
| 3- |
Self rating
depression scale (SDS) questionnaire (Zung scale) [17]: It is used for quantitative measurement of depression as an emotional disorder. It consists of 20 items. Each is related to a specific characteristic of depression. Opposite each statement, there are 4 columns headed none or a little of time, some of the time, part of the time, and most or all of the time. |
| Grading: |
|
< 50 = no depression.
50-59 = minimal to mild depression.
60-69 = moderate to marked
depression.
> 70 = severe to most extreme depression. |
| (E) |
Statistical analysis: |
| |
Results were expressed as mean + standard deviation (SD) or number (%). Comparison between two groups was performed using unpaired student t-test. Categorical data was compared using Chi-square test. Correlation between different parameters was performed using Pearson's rank correlation coefficient. Statistical analysis was performed with the aid of the statistical package for the social sciences (SPSS) computer program (version 10 windows). P value <0.05 was considered significant. |
Results:
The results of this study showed that the means of age and disease duration in vitiligo patients were 28.5+11.205 years and 9.58+7.66 years respectively, those of psoriasis patients were 38.2+12.827 years and 12.0+6.578 years respectively and those of AA patients were 26.58+9.533 years and 6.740+4.716 years respectively. Sex, social and working status of the three groups of patients is shown in
table (1) Table (1): Sex, social and working status in the 3 studied groups.
|
|
Vitiligo |
Psoriasis |
Alopecia areata |
Total |
|
Sex |
M |
*N |
25 |
25 |
28 |
78 |
|
% |
50 |
50 |
50 |
50 |
|
F |
N |
25 |
25 |
22 |
72 |
|
% |
50 |
50 |
50 |
50 |
|
Social status |
Unmarried |
N |
26 |
22 |
27 |
75 |
|
% |
52 |
44 |
54 |
50 |
|
Married |
N |
24 |
28 |
23 |
75 |
|
% |
48 |
56 |
46 |
50 |
|
Work |
Not working |
N |
22 |
24 |
17 |
63 |
|
% |
44 |
48 |
34 |
42 |
|
Working |
N |
28 |
26 |
33 |
87 |
|
% |
56 |
52 |
66 |
58 |
* N=Number Results of severity scoring in the 3 studied groups: In vitiligo patients, mean BSA% was 19.36 ± 10.88% (range: 4%-50%). Mean PASI score in psoriasis was 15.48 ± 7.16 (range: 3-30). In AA SALT score, 62% of patients were classified as S1, 28% as S2, 2% as S3, 2% as S4 and 6% as S5. Regarding B score, 74% of patients were categorized as B0 and 26% as B1. Pruritic symptoms were detected in a significantly higher percentage of psoriasis patients (50%) compared to AA (10%) and vitiligo (8%) patients (P<0.05).
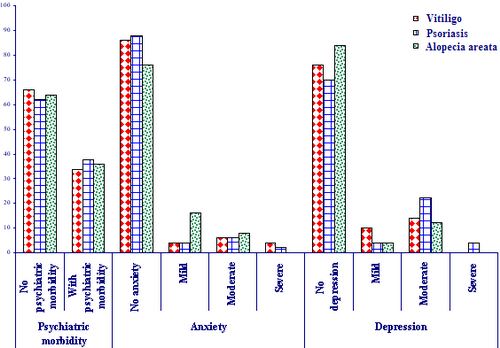
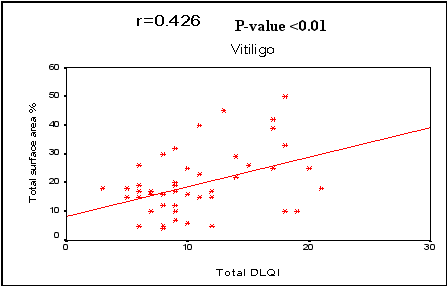
Relation of the 3 diseases to psychiatric morbidity, anxiety and depression
(Fig1): 1) Psychiatric morbidity: it was detected in 34% of vitiligo patients, 38% of psoriasis patients and 36% of AA patients.
2) Anxiety: it was detected in 14% of vitiligo patients, 12% of psoriasis patients and 24% of AA patients.
3) Depression: it was detected in 24% of vitiligo patients, 30% of psoriasis patients and 16% of AA patients. However, no statistically significant difference was found in 3 groups as regards psychiatric morbidity, anxiety or depression (P>0.05).
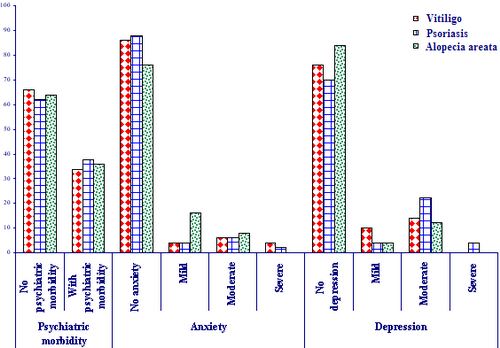
| Fig 1:
Relation of the three diseases to the psychiatric morbidity, anxiety
and depression. |
|
The mean age was found to be significantly higher in psychiatric morbidity negative patients in vitiligo and AA groups only (31.879+11.699 and 29.844+10.377 years respectively) compared to psychiatric morbidity positive cases (21.941+11.699 and 20.778+3.5 years respectively). On the other hand, in AA group only, married patients had significantly less psychiatric morbidity compared to unmarried patients (p<0.05). As regards mean disease duration, it was found to be significantly longer in psychiatric morbidity positive psoriasis patients (14.421+6.594) compared to that of psychiatric morbidity negative patients (10.516+ 6.212) (P<0.05). This relation was not statistically significant in the other 2 groups of patients. Clinical disease severity was significantly higher in psychiatric morbidity positive cases compared to psychiatric morbidity negative patients in the 3 studied groups (P<0.05) where mean BSA% in vitiligo patients was 26.235 ±12.068% versus 15.818 ± 8.394% respectively and mean PASI score in psoriasis patients was 21± 3.972 versus 12.097 ± 6.568 respectively. In AA, psychiatric morbidity was present in a higher percentage of patients with more severe disease grades. As regards the site of the disease, visible area involvement (face and hands) was significantly higher in psychiatric morbidity positive patients compared to psychiatric morbidity negative patients in vitiligo and psoriasis while other areas involved showed no significant relation to psychiatric morbidity in both diseases
(Table 2). Table (2): Psychiatric morbidity and its relation to the site of the disease in vitiligo and psoriasis:
|
Variables |
|
Psychiatric morbidity |
|
Disease groups |
No psychiatric morbidity |
ًWith psychiatric
morbidity |
Chi-square |
|
|
N |
% |
N |
% |
X2 |
P-value |
|
Face |
Vitiligo |
11 |
22 |
11 |
22 |
4.482 |
<0.05* |
|
Psoriasis |
2 |
4 |
10 |
20 |
13.773 |
<0.05* |
|
Hand |
Vitiligo |
14 |
28 |
12 |
24 |
3.566 |
<0.05* |
|
Psoriasis |
9 |
18 |
15 |
30 |
11.759 |
<0.05* |
|
Arms |
Vitiligo |
13 |
26 |
10 |
20 |
1.705 |
>0.05 |
|
Psoriasis |
27 |
54 |
19 |
38 |
2.665 |
>0.05 |
|
Trunk |
Vitiligo |
17 |
34 |
7 |
14 |
0.48 |
>0.05 |
|
Psoriasis |
11 |
22 |
12 |
24 |
3.632 |
>0.05 |
|
Genitalia |
Vitiligo |
13 |
26 |
8 |
16 |
0.271 |
>0.05 |
|
Psoriasis |
9 |
18 |
6 |
12 |
0.036 |
>0.05 |
|
Legs |
Vitiligo |
14 |
28 |
4 |
8 |
1.739 |
>0.05 |
|
Psoriasis |
26 |
52 |
14 |
28 |
0.764 |
>0.05 |
|
Feet |
Vitiligo |
17 |
34 |
9 |
18 |
0.009 |
>0.05 |
|
Psoriasis |
10 |
20 |
8 |
16 |
0.496 |
>0.05 |
* = significant X2=chi square N=Number In AA patients, out of the 36% of patients with psychiatric morbidity, 4% had single patches while 32% had multiple patches. Pruritic symptoms were detected in a significantly larger number of psoriasis patients with psychiatric morbidity (15 of total 19) than in those without psychiatric morbidity (10 out of 31) (P<0.05). This was not detected in the other 2 diseases. Suicidal thoughts occurred in 6% of vitiligo patients, 8% of psoriasis patients and 8% of AA patients while suicidal attempts occurred in 2% of vitiligo patients, 4% of psoriasis patients and 2% of AA patients. No statistically significant difference was detected between the 3 disease groups as regards sleep disturbance and suicidal attempts. However, mean age was significantly higher in sleep disturbance positive patients in the 3 diseases compared to sleep disturbance negative patients. Pruritus, likewise, showed a significant relation to sleep disturbance in psoriasis patients (P<0.05). Suicidal thoughts were significantly related to the disease severity in the 3 studied groups (P<0.05). In vitiligo, BSA% was significantly higher in patients with suicidal thoughts (29.333 ± 14.012) than in those without suicidal thoughts (18.723 ± 10.529). In psoriasis, the PASI score was also significantly more in patients with than those without suicidal thoughts (22 ± 5.958 versus 14.756 ± 6.965). Similarly, in AA, 3 patients had suicidal thoughts, 2 of them had S5 score. On the other hand, presence of suicidal thoughts showed no significant relation to demographic data or pruritus (P>0.05).
Comparison of QOL by DLQI and PCASEE in the 3 disease groups: The mean QOL by DLQI was significantly better in vitiligo and AA patients compared to that of psoriasis patients. However, by PCASEE, no statistically significant difference was found between the 3 diseases (Table 3).
Table (3): Comparison of quality of life by DLQI and PCASEE in the three diseases of the study:
|
|
Vitiligo |
Psoriasis |
Alopecia areata |
ANOVA |
|
f |
P-value |
|
Total DLQI |
Range |
3.0-21.0 |
4.0-27.0 |
2.0-20.0 |
8.803 |
<0.05* |
|
Mean |
10.86 |
13.68 |
9.06 |
|
SD |
4.499 |
6.814 |
5.073 |
|
groups |
V & P |
V & A |
P & A |
|
Turkey's test |
0.030* |
0.236 |
<0.001* |
|
Total score PCASEE |
Range |
60-120 |
60-126 |
55-130 |
1.22 |
>0.05 |
|
Mean |
96.4 |
93.9 |
99.72 |
|
SD |
16.97 |
18.84 |
20.11 |
* = significant Relation of DLQI and PCASEE to psychiatric morbidity, anxiety, depression and severity of the diseases: In the 3 diseases, the mean score of QOL by both DLQI and PCASEE was significantly worse in psychiatric morbidity positive patients than psychiatric morbidity negative patients
(Table 4). Table (4): Relation of quality of life by DLQI to psychiatric morbidity in the three dermatological diseases of this study.
|
Total DLQI |
Psychiatric morbidity |
|
No psychiatric morbidity |
Psychiatric morbidity |
T-test |
|
Mean |
± |
SD |
Mean |
± |
SD |
t |
P-value |
|
Vitiligo |
8.152 |
± |
2.152 |
16.118 |
± |
2.87 |
-11.05 |
<0.05* |
|
Psoriasis |
9.806 |
± |
4.792 |
20 |
± |
4.485 |
-7.477 |
<0.05* |
|
Alopecia areata |
6.406 |
± |
2.917 |
13.778 |
± |
4.672 |
-6.88 |
<0.05* |
* = significant SD=Standard deviation There was a significant relation between poorer QOL and depression and anxiety in the 3 disease groups by both DLQI
(Tables 5&6) and PCASEE (Tables 7&8). Table (5): Relation of quality of life by DLQI with anxiety in the three dermatological diseases of this study.
|
Total DLQI |
Anxiety |
|
Negative |
Positive |
T-test |
|
Mean |
± |
**SD |
Mean |
± |
SD |
t |
P-value |
|
Vitiligo |
10.023 |
± |
4.149 |
16 |
± |
3 |
-3.645 |
<0.05* |
|
Psoriasis |
12.432 |
± |
6.226 |
22.833 |
± |
2.714 |
-4.012 |
<0.05* |
|
Alopecia areata |
8.125 |
± |
4.794 |
12.8 |
± |
4.59 |
-2.78 |
<0.05* |
* = significant SD=Standard deviation
Table (6): The relation of quality of life by DLQI to depression in the three dermatological disorders studied
|
Total DLQI |
Depression |
|
Negative |
Positive |
T-test |
|
Mean |
± |
SD |
Mean |
± |
**SD |
t |
P-value |
|
Vitiligo |
9.026 |
± |
3.149 |
16.667 |
± |
2.902 |
-7.456 |
<0.05* |
|
Psoriasis |
11.114 |
± |
5.835 |
19.667 |
± |
4.995 |
-4.946 |
<0.05* |
|
Alopecia areata |
8 |
± |
4.265 |
16.833 |
± |
3.656 |
-4.827 |
<0.05* |
* = significant SD=Standard deviation Table (7): Relation of quality of life by PCASEE to anxiety in the three dermatological diseases of this study
|
Total score of PCASEE |
Anxiety |
|
No anxiety |
With anxiety |
T-test |
|
Mean |
± |
SD |
Mean |
± |
**SD |
t |
P-value |
|
Vitiligo |
98.326 |
± |
18.299 |
77.429 |
± |
9.271 |
2.942 |
<0.05* |
|
Psoriasis |
96.955 |
± |
17.713 |
71.5 |
± |
9.813 |
3.428 |
<0.05* |
|
Alopecia areata |
102.4 |
± |
23.484 |
79 |
± |
8.692 |
3.078 |
<0.05* |
* = significant SD=Standard deviation
Table (8): Relation of quality of life by PCASEE to depression in the three dermatological diseases of this study
|
Total score of PCASEE |
Depression |
|
No depression |
With depression |
T-test |
|
|
Mean |
± |
SD |
Mean |
± |
SD |
t |
P-value |
|
Vitiligo |
101.95 |
± |
16.19 |
74.667 |
± |
8.105 |
5.591 |
<0.05* |
|
Psoriasis |
101.6 |
± |
16.849 |
75.933 |
± |
7.676 |
5.629 |
<0.05* |
|
Alopecia areata |
101.43 |
± |
22.15 |
70.5 |
± |
9.16 |
3.357 |
<0.05* |
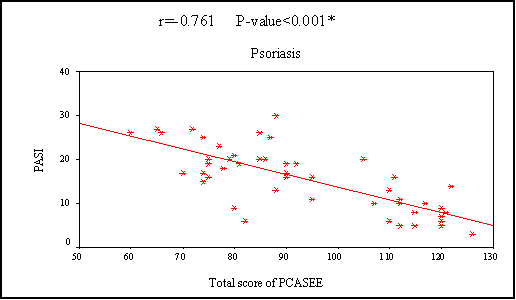
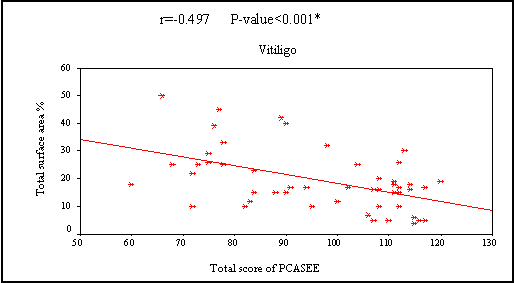
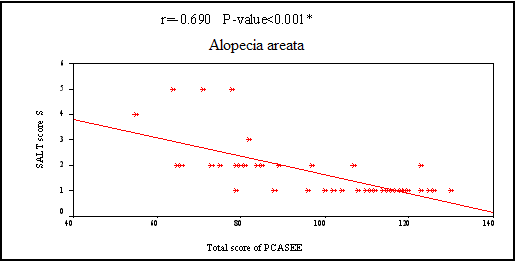
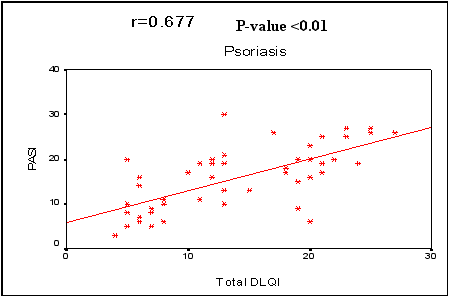
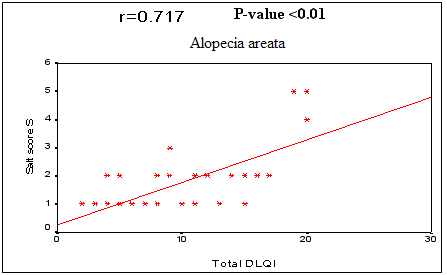
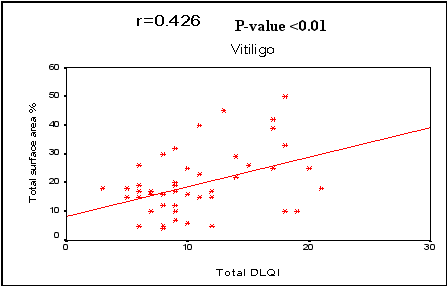
* = significant SD=Standard deviation In the 3 diseases, QOL showed a statistically significant negative correlation by PCASEE and a statistically significant positive correlation by DLQI with disease severity
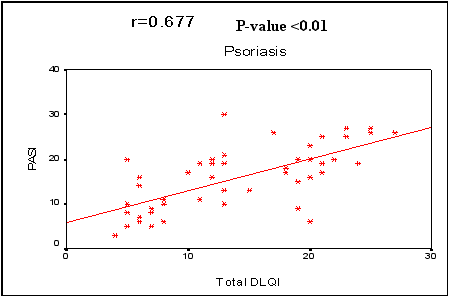
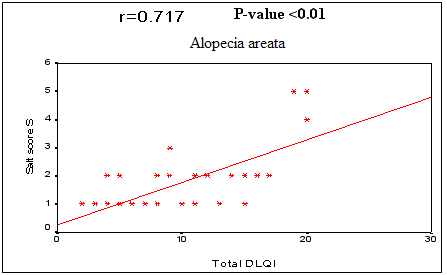
(Fig 2 a&b).
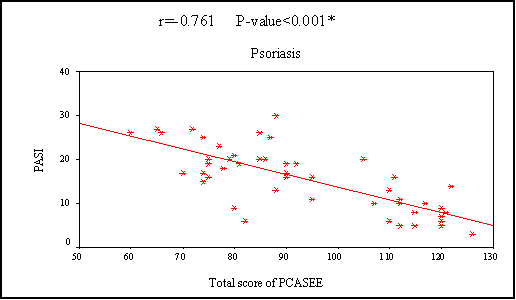
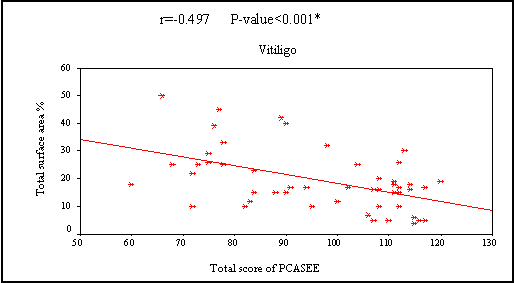
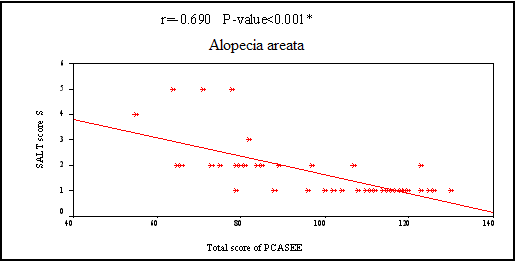
| Fig. (2a): Correlation between the severity of the three diseases and quality of life by PCASEE |
|
|
Fig (2b): Correlation between severity of the three diseases and quality of life by DLQI. |
|
Discussion:
The last decade has witnessed an increasing interest in psychological effects of various skin diseases and QOL in patients suffering from these diseases [18]. So, in this work, a study of psychiatric morbidity and QOL in vitiligo, psoriasis and alopecia areata was done as these are common cosmetically disfiguring dermatological conditions. In this study, psychiatric morbidity was found in 34% of vitiligo patients, 38% of psoriasis patients and 36% of AA patients. Anxiety was detected in 12% of vitiligo patients, 10% of psoriasis patients and 24% of AA patients while depression was found in 22% of vitiligo patients, 28% of psoriasis patients and 14% of AA patients. Four percent of each group of patients had both anxiety and depression. On reviewing the literature, there were no studies comparing psychiatric morbidity and QOL in the three studied diseases. However, in studies for the psychiatric morbidity in vitiligo and psoriasis, it was found that the prevalence of psychiatric co-morbidity was 16-34% in vitiligo and that in psoriasis was 29-53%. Vitiligo patients had depression episodes (18-22%), depression (10%) and anxiety (3.3%) [19,20]. These results are therefore matching with the results of this study. However, in other studies on psoriasis patients with psychiatric morbidity, the percentages of patients with depression and anxiety on standardized psychiatric diagnosis were higher than those detected in our study (50-97% and 15-50% respectively)[21,22]. Jowett and Ryan (1985)[23] found that 24% of psoriasis patients had depression and 58% suffered from anxiety. Mattoo et al. (2005)[19] found 22.33% rate of psychiatric disorders. The profile of psychiatric diagnosis was 65% adjustment disorder depressed type, 30% depressive episodes and 4% dysthemia. However, no anxiety disorders were detected in their study. Previous studies on AA patients showed variable results varying from 66 %[24] to 93 %[25] psychiatric illness. Other studies found that the degree of anxiety among AA patients was not greater than control [26,27]. The difference in the prevalence of anxiety and depression in different studies could be due to difference in diagnostic systems used. In addition, different methodology such as patients' recruitment and difference in population characters make the comparison between these studies difficult. In this study, younger patients were more prone to have psychiatric morbidity but the statistically significant difference was for vitiligo and AA patients. Duration of the three diseases was longer in psychiatric morbidity positive patients but it was statistically significant in psoriasis only. Unmarried patients in AA had a statistically significant difference compared to other disease groups as regards psychiatric morbidity. These results denote that unestablished social life in younger and unmarried patients makes them worry about their future resulting in more psychological distress and psychiatric morbidity. The current study revealed that in psychiatric morbidity positive psoriasis patients, pruritus was significant. It was found to be insignificant in the other two diseases. Other reports considered pruritus as a significant predictor of depression in psoriasis patients and its improvement after treatment results in improvement of depression [28,29]. This also supports the fact that psychiatric morbidity patients are more burdened by symptoms as found in our psoriasis patients but they do not perceive non existing symptoms [30], as found in our vitiligo and AA patients. We found that the severity of the three diseases had significant relations to psychiatric morbidity. This was previously reported in psoriasis [31] and AA [23]. Other studies found social stigmatization to correlate more with psychiatric morbidity in vitiligo and psoriasis[32,33]. In our study, disease severity profoundly affected our patients, gave them hopeless feeling that their skin condition will not improve especially with their bad life circumstances and low economic support for treatment. The present study showed that psychiatric morbidity was related in vitiligo and psoriasis patients to presence of lesions in a visible area which leads to more stigmatization and in AA patients to presence of multiple patches. This implies that the effect of those diseases on the look of the patients is psychologically distressing. Ongenae et al. (2005)[33] found that patients with lesions in visible areas were more burdened with their vitiligo, and in psoriasis Krueger et al. (2000)[34] found that visible area involvement resulted in more impact on patients' life than involvements of the same size in other invisible areas. In AA, our results were generally in agreement with Ruiz-Doblado et al. (2003) [24]. Suicidal ideation is a serious problem among sufferers of these disfiguring dermatological diseases. This study showed 8% rate of suicidal ideation in psoriasis patients. In a study by Gupta et al. (1993)[35], psoriasis patients had 9.7% prevalence of suicidal thoughts and 5.5% suicidal attempts, which is slightly more than that in our study (4%). They found that a higher disease severity in psoriasis was associated with a higher prevalence of suicidal ideation. Similarly we found that the severity of the three dermatological diseases had a significant relation to suicidal ideation. To the best of our knowledge, there are no studies about suicidal ideation in vitiligo but compared to psoriasis, we found that they had lower prevalence (6%) but the same prevalence as in AA. Suicidal attempts were less (2%). Gupta and Gupta (1998) [36], found that 9.1% of AA patients thought that it was better if they were dead. These rates are two fold greater than those found in the general community [37]. The nearly similar results in the suicidal ideation in the three dermatological diseases in this study may be due to similar prevalence of psychiatric morbidity among them. Psoriasis patients who had more pruritic symptoms suffered more from sleep disturbance. Gupta et al. (1993) [35], highlighted the link between suicide and depression and sleep disturbance. Gupta et al. (1988) [38], found that the pruritus is significantly related to sleep disturbance and suicidal thoughts. In this study, the QOL of patients was measured by two standard measures, one is generic PCASEE [10] and the second is the DLQI which specifically measures the effects of the dermatological diseases on the QOL of the patients [12]. QOL by DLQI in our vitiligo patients was worse compared to that of Belgian patients [33]. This might be due to the lighter skin color of the Belgian patients that cause less cosmetic disfigurement and the better facilities for treatment compared to our patients. On the other hand, a study on Indian patients showed comparable results to ours may be because of the similar conditions including dark skin color and the quality medical services. Our psoriasis patients similarly showed a worse QOL by DLQI if compared to Belgian patients [33]. This could be explained by lower clinical severity in that study compared to a higher mean severity of the disease in our patients, thus implying a great impact of higher disease severity on QOL. QOL in AA patients by DLQI was less impaired than vitiligo and psoriasis patients. This could be attributed to the fact that in our Islamic country, most of the females cover their hair and also small patches may not be noticed. As for males, they can shave their hair in order not to make the site of the patches apparent. We did not find other studies on the QOL in AA using DLQI. Psoriasis had the worst QOL compared to the other 2 studied diseases as the patients' burden from subjective symptoms such as physical disability, bleeding and pruritus is more than the other 2 diseases. We found a strong association between psychiatric morbidity and poorer QOL in the skin diseases using both PCASEE and DLQI. Sampogna et al. (2004) [39] observed similar results not only with these diseases but also with a wide range of other skin diseases. The results of this study are of particular interest as they represent typical problems encountered by dermatologists in their practice. Thus, dermatological patients with concurrent psychiatric disorders need particular attention realizing the increased burden of the disease on their quality of life. A mutual respectful collaboration between dermatological and mental health professionals might be of help for many patients. There are studies documenting that not only emotional distress, but also skin lesions themselves can be ameliorated by psychotherapeutic intervention [40,41]. Dermatologists should evaluate the psychosocial stress caused by the disease by simple questions or standardized questionnaires. The role of psychiatric intervention in dermatological patients with vitiligo, psoriasis and AA should be further evaluated to determine its effect on QOL related to these three common diseases. In addition, studies including control subjects and larger patient groups are needed to verify or refute these results. In conclusion, it is important for dermatologists to understand the profound effect of these diseases on the QOL and to know the psychosocial and psychiatric consequences of the diseases. Although the diseases studied are not considered to be life threatening, the dermatologist should consider them as serious. This may help in selecting the suitable type of treatment. References
1. Porter J, The psychological effects of vitiligo: response to impaired appearance. In: Vitiligo a Monograph on the Basic and Clinical Science. Hann Sk, Nordlund JJ, eds Blackwell Science, Oxford, 97-100, 2000.
2. Picardi A and Abeni D, Stressful life events and skin diseases: disentangling evidence form myth, Psychother Psychosom. 70: 118-136, 2001.
3. Medansky RS and Handler RM, Dermatopsychosomatics: classification, physiology, and therapeutic approaches, J Am Acad Dermatol. 5: 125-36, 1981.
4. Mease J and Menter M, Quality of life issues in psoriasis and psoriatic arthritis: Outcome measures and therapies from a dermatological perspective. J Am Acad Dermatol. 54: 685-704, 2006.
5. Gupta MA and Gupta AK, Psychodermatology: an update, J Am Acad Dermatol. 34: 1030-46, 1996.
6. Finlay AY and Ryan TJ, Disability and handicap in dermatology, Int J Dermatol. 35: 305-311, 1996.
7. Fredriksson T and Pehersson U, Severe psoriasis oral therapy with a new retinoid, Dermatologica. 157: 238-244, 1978.
8. Olsen E, Hordinsky M, McDonald-Hull SP, Price V, et al., Alopecia areata investigational guidelines, J Am Acad Dermatol. 40: 242-246, 1999.
9. Kanthraj GR, Srinivas CR, Shenoi SD, Deshmukh RP, Suresh B, Comparison of computer- aided design and rule of nines methods in the evaluation of the extent of body involvement in cutaneous lesions, Arch Dermatol. 133(7): 922-923, 1997.
10. Bech P, Quality of life instruments in depression, European Psychiatry. 12: 194- 199, 1996.
11. Sadek A, Omera Z, Ramy HEL and Sabary M, Quality of life of schizophrenic and mood disorder patient. Role of day center. MD thesis, faculty of medicine, ASU. 2003
12. Finaly A and Khan G, Dermatology life quality index (DLQ1): A simple practical measure for routine clinical use, Clin Exp Dermatol.; 19: 210-216, 1994.
13. Goldberg DP and Hiller VS, Scaled version of the General Health Questionnaire, Psychol Med. 9: 139- 145, 1979.
14. Okasha A, Kamel M, Fares R et al., An epidemiological study of depressive symptom in rural and urban population in Egypt, Egypt J Psychiat. 11: 45- 54, 1988.
15. Taylor J, A Personality Scale of Manifest Anxiety, J Abnorm Psychol. 48 (2): 258- 90, 1953.
16. Fahmi M, Ghali M and Meleka K, Arabic version of the personality scale of manifest anxiety, Egyptian Psychiatry. 11: 119- 126, 1977.
17. Zung WW, Self-Rating depression Scale, Arch Gen Psychiatry. 12: 63- 70, 1965.
18. Mehto V and Malhotre SK, Psychiatric evaluation of patients with psoriasis vulgaris and chronic urticaria, German J Psychiatry. 10: 104- 110, 2007.
19. Mattoo SK, Handa S, Kaur I, Gupta N and Malhotra R, Psychiatric morbidity in vitiligo: prevalence and correlates in India, J Eur Acad Dermatol Venereol.; 16: 573- 578, 2005.
20. Sharma N, Koranne RV and Singh RK, Psychiatric morbidity in psoriasis and vitiligo: a comparative study, J Dermatol. 28: 419- 423, 2001.
21. Mummer S, Tuba A, Yelda K and Hamdi O, Psychiatric morbidity in dermatology patients: Frequency and results of consultations, Indian J Dermatol. 51: 18- 22, 2006.
22. Deshapande N, Desai N, Mundra V K et al., Psychiatric aspect of psoriasis, Arch Ind Psychiatry. 61-64, 1998.
23. Jowett S and Ryan T, Skin disease and handicap: an analysis of the impact of skin conditions, Soc Sci Med. 20(4): 425- 429, 1985.
24. Ruiz-Doblado S, Carrizosa A and Garcia-Hernandez MJ, Alopecia areata: Psychiatric comorbidity and adjustment to illness, Int J Dermatol. 42: 434- 437, 2003.
25. Greenberg SI, Alopecia Areata: a psychiatric survey, Arch Dermatol. 72: 454-457, 1955.
26. Paga G, Faina P, Teodori A et al., Psychological factors in alopecia areata: results from a preliminary, controlled study, New Trends Exp Clin Psychiatry. 8:73- 79, 1992.
27. Gupta MA and Gupta AK, Psoriasis and sex: a study of moderately to severely affected patients, Int J Dermatol. 36: 259- 62, 1997.
28. Gupta MA, Gupta AK, Kirkby S, et al., Pruritus in psoriasis: a prospective study of some psychiatric and dermatologic correlates, Arch Dermatol. 124: 1052-1057, 1988.
29. Gupta MA, Gupta AK, Schork NJ, et al., Depression modulates pruritus perception: a study of pruritus in psoriasis, atopic dermatitis, and chronic idiopathic urticaria, Psychosom Med. 56: 36- 40, 1994.
30. Devrimici-Ozguven H, Kundakci N, Kumbaser H and Boyvat A, The depression, anxiety life satisfaction and affective expression levels in psoriasis patients, J Eur Acad Dermatol Venereol. 14: 267- 71, 2000.
31. Zachariae R, Zachariae H, Blomqvist K, et al., Quality of life in 6497 Nordic patients with psoriasis, Br J Dermatol. 146: 1006- 1016, 2002.
32. Gupta MA and Gupta AK, Psychiatric and psychological co-morbidity in patients with dermatologic disorders: epidemiology and management, Am J Clin Dermatol. 4: 833- 842, 2003.
33. Ongenae K, Van Geel N, De Schepper S and Naeyaert JM, Effect of vitiligo on self-reported health-related quality of life, Br J Dermatol. 152: 1165- 1172, 2005.
34. Krueger GG, Feldman SR, Camisa C, et al., Two considerations for patients with psoriasis and their clinicians: What define mild, moderate and severe psoriasis? What constitutes a clinically significant improvement when treating psoriasis? J Am Acad Dermatol. 43: 281- 285, 2000.
35. Gupta MA, Gupta AK, Schork NJ, et al., Suicidal ideation in psoriasis, Int J Dermatol. 32: 188- 190, 1993.
36. Gupta MA and Gupta AK, Depression and Suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis, Br J Dermatol. 139(5): 846- 850, 1998.
37. Olfoson M, Lewiss-Feranndez R, Wissmman MM, et al., Psychotic symptoms in an urban general medicine practice, Am J Psychiatry. 159: 1412- 19, 2002.
38. Gupta AM, Gupta AK, Kirkby S et al., Pruritus in psoriasis: a prospective study of some psychiatric and dermatologic correlates, Arch Dermatol. 124: 1052-1057, 1988.
39. Sampogna F, Picardi A, Chren M, et al., Association between poorer quality of life and psychiatric morbidity in patients with different dermatological conditions, Psychosomatic Medicine. 66: 520- 526, 2004.
40. Kabat-Zinn J, Wheeler E, and Light T et al., Influence of a mindfulness mediation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA), Psychosom Med. 60: 625- 632, 1998.
41. Papadopulous L, Bor R and Legg C, Coping with the disfiguring effects of vitiligo: a preliminary investigation into the effects of cognitive-behavioural therapy, Br J Med Psychol. 72: 385- 396. 1999.
الملخص
العربي
دراسة مقارنة للمرض النفسي و نوعية الحياة في
مرض الصدفية و البهاق والحاصة البقاعية
حنان محمد صالح* ، سمر عبد الله سالم* ، رانيا الششتاوى * و عفاف محمد عبد
السميع**
قسم الأمراض الجلدية والتناسلية* وقسم الأمراض النفسية والعصبية**
كلية طب جامعة عين شمس
لقد زاد الاهتمام في العقد الأخير بالتأثير النفسي للمرض
الجلدي وتأثيره على طبيعة حياة المريض.
هدف البحث هو تقييم مدى تأثير المرض النفسي ونوعية الحياة في
الأمراض الجلدية الثلاثة (الصدفية ، والبهاق والحاصة البقاعية) لدى المرضى
المصريين الذين يترددون على عيادة الجلدية الخارجية كلية طب جامعة عين شمس.
ويضم هذا البحث 150 مريضا (50 مريضا بالصدفية ، 50 مريض
بالبهاق و 50 مريضا بالحاصة البقاعية) وتم تقييم نوعية الحياة للمريض عن طريق
مقياس “PCASEE”
ومقياس الجلدي لنوعية الحياة وكذلك تقييم المرض النفسي بواسطة اختبار الصحة
العامة وتقييم الإضطرابات النفسية بواسطة استخدام مقياس تيلر لتقييم القلق
النفسي واستخدام مقياس زونج لتقييم الأكتئاب.
وقد وجدنا أن 34% من مرضى البهاق ، 38% من مرضى الصدفية و36%
من مرضى الحاصة البقاعية يعانون من المرض النفسي ، ويعانى 14% من مرضى البهاق
، 12% من مرضى الصدفية و 24% من مرضى الحاصة البقاعية من التوتر النفسي ،
بينما يعانى أولئك المرضى من الأكتئاب بنسبة 24% من مرضى البهاق ، 30% من مرضى
الصدفية و16% من مرض الحاصة البقاعية. وقد وجد أن زيادة شدة المرض يزداد معها
أعراض المرض النفسي والتأثير على نوعية الحياة وقد يكون ذلك نتيجة للتأثير
المتبادل بين المرض الجلدي والمرض النفسي.
ونستنتج من هذا البحث أن أمراض الصدفية والحاصة البقاعية
والبهاق مرتبطة بوجود مرض نفسي ووجود علاقة قوية بين المرض النفسي ونوعية
الحياة وتأثيرها على هذه الأمراض الجلدية وأنه من المهم والضروري أن يتفهم طبيب
الأمراض الجلدية التأثير العميق لهذه الأمراض الجلدية على حالة المريض النفسية
وعلى طبيعة حياته ويجب علاج هذه الأمراض بكل الوسائل ويجب متابعة تأثير العلاج
النفسي سواء الدوائي أو السيكولوجي على المريض وتأثير ذلك على تحسن حالته
المرضية الجلدية
© 2008 Egyptian Dermatology Online Journal |