|
|
Abstract
A 26-year-old female patient was referred to us for skin lesions mainly over extensor surfaces of limb joints and ear lobes of two-week duration. Patient was under evaluation as an in-patient in the department of internal medicine for recurrent polyarthritis and fever. A skin biopsy from the lesion demonstrated a neutrophilic vasculitis and blood investigations significantly showed a pANCA (Peripheral Anti-Neutrophilic Cytoplasmic Antibody) and rheumatoid factor positivity. A diagnosis of Erythema Elevatum Diutinum (EED) was considered based on the clinical features and investigation results. We present this a case of EED with vesicular lesions associated with rheumatoid arthritis and pANCA positivity. Case report:
A 26-year-old female patient, being treated as an in-patient under internal medicine was referred to us for raised skin lesions over multiple areas of the body of two weeks duration. Her complaints had started as fever and joint pains associated with raised skin lesions mainly over the elbows, knees, ankles and ear lobes [Fig1,
Fig2 and Fig3]. There was no significant itching, burning or pain. The fever was high grade and intermittent. Joint involvement was limited to elbow joints, knee joints and small joints of fingers. She had no history of any mucosal lesions or epistaxis. She did not complain of any respiratory difficulties, dysuria, vomiting, diarrhoea or abdominal pain. There was no history suggestive of any bleeding
tendencies. The patient did not give a history of any visual problems.
 | Fig 1:
Vesicles, papules, papulo-vesicles and nodules on the right elbow |
|
 | Fig
2: Vesicular lesions on the right ear lobe |
|
 | Fig
3: Vesicles over left ear lobe |
|
In the past (9 years ago) she had been evaluated for an episode of fever, arthritis and skin rash which was then diagnosed as systemic vasculitis and had been treated with oral steroids for 3 years. Since then she had had intermittent episodes of arthritis with significant morning stiffness and skin rashes mainly over the extensor aspects. All her symptoms had been relatively well controlled with non-steroidal anti-inflammatory drugs along with intermittent steroids. There was no past history of seizures or cardiac problems. There was no personal or family history of tuberculosis, bronchial asthma, hypertension or diabetes mellitus. On dermatological examination grouped erythematous papules, nodules and vesicles with minimal crusting were seen mainly over the elbow joints, knee joints, ankles, lower legs, dorsum of hands and ear lobes. The vesicular lesions were tense and clear. There were no evident hemorrhagic vesicles. There was no evidence of mucosal involvement. Scalp, hair, nails, palms and soles were normal. A clinical diagnosis of cutaneous vasculitis was considered, the primary differential for the cutaneous lesions being erythema
elevatum diutinum. The other differentials considered included rheumatoid neutrophilic
dermatosis , rheumatoid vasculitis, non-specific ANCA positive vasculitis and atypical
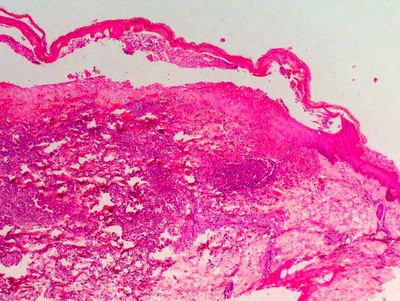
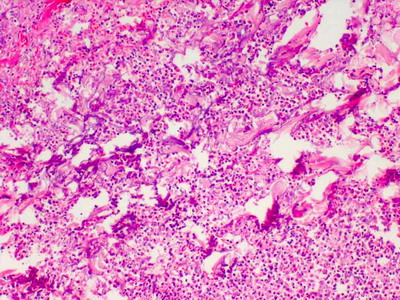
pyoderma gangrenosum. However, the distribution of the lesions was more in favour of EED. Rheumatoid arthritis was considered as the primary systemic diagnosis (The diagnosis of EED mainly being based on the nature and distribution of the lesions, and the known association of EED with rheumatoid arthritis and vasculitis). A skin biopsy demonstrated a prominent neutrophilic vasculitis with subepidermal clefting in the specimen taken from the vesicular area
[Fig4 and Fig5]. There was no evidence of granulomatous inflammation. Direct immuno-fluorescence was negative.
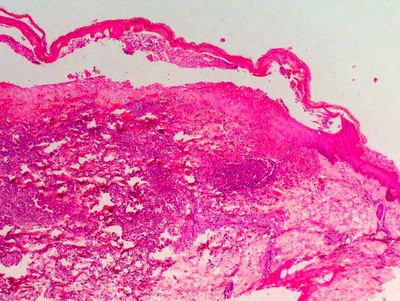 | Fig
4: Histopathology (H&E 20X) showing sub-epidermal with dermal neutrophilic
infiltration |
|
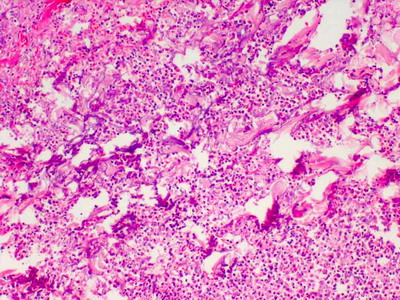 | Fig
5: Histopathology (H&E X100) showing pan-dermal neutrophilic
infiltration with focal leukocytoclastic vasculitis |
|
Blood results showed revealed significant anaemia (haemoglobin count was 6.2 g/dl at the time of admission), raised erythrocyte sedimentation rate (80mm at time of admission) strongly positive rheumatoid factor and a positive p-ANCA. Antinuclear antibody profile and cANCA were negative. Chest radiography was normal. Electro-Cardio-Gram showed normal sinus rhythm. Ultrasound of the abdomen and pelvis showed a mild hepatomegaly. Serum electrophoresis was normal. Widal test was negative. Blood culture and urine culture did not show any growth. Leptospira IgM Elisa, Dengue virus IgM Elisa, Paul-Bunnel test and Chikungunya IgM rapid test were all negative. Peripheral smear showed a microcytic, hypochromic, anemia with neutrophilic leukocytosis and thrombocytosis. VDRL, HIV 1 & 2 antibody, HBsAg, and antiHCV screen was negative.Cardiac Echo and bone marrow examination were also
done, both of which were normal. Finally based on the clinical, histological and laboratory findings a diagnosis of Erythema Elevatum Diutinum associated with Rheumatoid Arthritis was made. The severe anaemia was attributed to chronic rheumatoid arthritis as bone marrow and electrophoresis findings were normal.
Patient was started on injectable methylprednisolone and hydroxychloroquine along with supportive measures - iron supplementation and non-steroidal anti-inflammatory drugs.
The patient showed good response with complete remission of skin lesions and significant improvement in articular symptoms at time of discharge
for a further follow up after a month. Discussion:
Erythema Elevatum Diutinum (EED) is chronic cutaneous vasculitis occurring in association with a variety of conditions including autoimmunity, infectious disease, and hematological abnormalities. The role of associated medical problems is controversial, and the exact pathogenesis of EED is unknown although an Arthus-type reaction to bacterial and viral antigens has been suggested [1] The typical clinical presentation is described as erythematous papules and plaques involving the extensor surfaces of the extremities. Histologically, a spectrum from leukocytoclastic vasculitis to vessel occlusion and dermal fibrosis can be seen. The lesions of EED have many mimics clinically and histologically [2,3]. Establishing the diagnosis of EED is important so appropriate screening for associated conditions can ensue. Erythema elevatum diutinum has been associated with several immunological and infectious diseases such as recurrent / chronic bacterial infection (esp. streptococcal), HIV, collagen vascular diseases (rheumatoid arthritis, relapsing polychondritis, lupus erythematosus), haematological disorders (hypergammaglobulinemia, multiple myeloma, myelodysplasia), inflammatory bowel disease, B-cell lymphomas, myeloproliferative disorders and gout [4,5]. Immuno-histochemical studies have demonstrated that the vascular endothelium of EED stains positive for CD31, CD34, VEGF (Vascular Endothelial Growth Factor ), and factor VIIIa and negative for factor XIIIa, and TGFB (Transforming Growth Factor Beta), a reaction pattern that does not distinguish it from similar appearing lesions. Thus, the chronic and recurrent nature of EED is the primary means of distinguishing it from entities that are clinically and histologically similar [6] Vesiculobullous lesions have been reported in EED, though this is very rare [1,7]. To the best of our knowledge there is no specific report of vesicular EED occurring in the context of rheumatoid arthritis. Various treatment options have been tried in EED including dapsone [8], systemic corticosteroids, tetracycline, niacinamide [7], sulfapyridine and colchicine. EED associated with paraproteinemia has been reported to respond to intermittent plasma exchange [9]. Vesicular lesions histologically showing neutrophilic vasculitis, over extensor surfaces have been described in various ANCA positive
vasculitis like Wegener's granulomatosis and microscopic polyangiitis [10]. However in our case there was no other clinical evidence to suggest a primary ANCA positive
vasculitis. Hence ANCA positivity might have been only a non-specific incidental finding. Moreover ANCA positivity has been well documented in rheumatoid arthritis [11,12,13] as well as in EED itself [14]. The other possible diagnosis to be thought of in this case would be
rheumatoid neutrophilic dermatosis which is a rare cutaneous manifestation of
rheumatoid arthritis and can present with erythematous papules, purpuric
lesions, nodules and pustular lesions. The common sites affected include the trunk shoulders and neck .[15] We present this case to highlight the possibility of EED in patients presenting with vesicular lesions and also to consider the possibility of EED in patients presenting with vesicular lesions in the setting of rheumatoid arthritis and ANCA positivity. References
1.
Tomasini C, Seia Z, Dapavo P, Soro E, Addese C, Pippione M. Infantile
erythema elevatum diutinum: report of a vesiculo-bullous case. Eur J
Dermatol 2006; 16: 683- 6.
2.
Yiannias JA, el-Azhary RA, Gibson LE. Erythema elevatum diutinum: a clinical
and histopathologic study of 13 patients. J Am Acad Dermatol 1992; 26: 38-
44 .
3.
Wilkinson SM, English JS, Smith NP, Wilson-Jones E, Winkelmann RK. Erythema
elevatum diutinum: a clinicopathological study. Clin Exp Dermatol 1992; 17:
87- 93.
4.
Sachdev DS, Kharkar VD, Mahajan SA, Gupte PD. Erythema elevatum diutinum. J
Postgrad Med 2002; 48: 310-1.
5.
Muscardin LM, Cota C, Amorosi B, Ferraro C. Erythema elevatum diutinum in
the spectrum of palisaded neutrophilic granulomatous dermatitis: description
of a case with rheumatoid arthritis. J Eur Acad Dermatol Venereol 2007; 21:
104- 5.
6.
Wahl CE, Bouldin MB, Gibson LE. Erythema elevatum diutinum: clinical,
histopathologic, and immunohistochemical characteristics of six patients. Am
J Dermatopathol 2005; 27: 397- 400.
7.
Kohler IK, Lorincz AL. Erythema elevatum diutinum treated with niacinamide
and tetracycline. Arch Dermatol 1980; 116: 693- 5.
8.
Katz SI, Gallin JI, Hertz KC, Fauci AS, Lawley TJ. Erythema elevatum
diutinum: skin and systemic manifestations, immunologic studies, and
successful treatment with dapsone. Medicine (Baltimore). 1977; 56: 443- 55.
9.
Chow RKP, Benny WB, Coupe RL, Dodd WA, Ongley RC. Erythema elevatum diutinum
associated with IgA paraproteinemia successfully controlled with
intermittent plasma exchange. Arch Dermatol 1996; 132: 1360- 63.
10.
Peñas PF, Porras JI, Fraga J, Bernis C, Sarriá C, Daudén
E. Microscopic polyangiitis. A systemic vasculitis with a positive P-ANCA.
Br J Dermatol. 1996 ;134:542-7.
11.
Manolova I, Dantcheva M. Antineutrophil cytoplasmic antibodies in Bulgarian
patients with rheumatoid arthritis: characterization and clinical
associations. Rheumatol Int 2005; 26: 107- 14.
12.
Mulder AH, Horst G, van Leeuwen MA, Limburg PC, Kallenberg CG.
Antineutrophil cytoplasmic antibodies in rheumatoid arthritis.
Characterization and clinical correlations. Arthritis Rheum 1993; 36: 1054-
60.
13.
Bosch X, Llena J, Collado A, Font J, Mirapeix E, Ingelmo M, et al.
Occurrence of antineutrophil cytoplasmic and antineutrophil (peri)nuclear
antibodies in rheumatoid arthritis. J Rheumatol 1995; 22: 2038- 45.
14.
Ayoub
N, Charuel JL, Diemert MC, Barete S, André M, Fermand JP, et al.
Antineutrophil cytoplasmic antibodies of IgA class in neutrophilic
dermatoses with emphasis on erythema elevatum diutinum. Arch Dermatol 2004;
140: 931- 6
15.
Magro CM, Crowson AN. The spectrum of cutaneous lesions in rheumatoid
arthritis: a clinical and pathological study of 43 patients. J Cutan Pathol
2003; 30: 1-10
© 2009 Egyptian Dermatology Online Journal |