|
|
Abstract:
It is a rare condition characterised by the
infiltration of skin by leukemic cells before their appearance in the
peripheral blood or bone marrow. We report a case of aleukemic leukemia
cutis in a fit gentleman, who rapidly progressed to acute myeloid leukomia.
However, the outcome was fatal within 3 months of diagnosis of skin lesions.
Case Report:
An 82 year old retired policeman was referred to
dermatology department with several weeks' history of a symptomatic
generalised erythematous papulo-nodular
rash on face, upper limbs,
trunk, and lower limbs
following a flu jab.
He had a past medical history of asthma and
hypertension and he was on ibesartan and salbutamol inhaler. There was no
improvement following oral and topical steroid and also changing his
antihypertensive medication Ibesartan to doxazocin by his GP.
On examination he looked very well with no lymphadenopathy or organomegally. The rash (Fig 1a, 1b,
1c, 1d) was reddish-purple infiltrative, firm,
papulo-nodular lesions about 0.5 to 1.5 cm in diameter with a smooth
surface on the torso and proximal parts of the extremities. All blood tests
including full blood counts, erythrocyte sedimentation rate, liver and renal
functions tests, blood film, autoantibody
screen and X-ray chest were normal.
 |
Fig 1a:
Leukaemia cutis affecting the trunk |
|
 |
Fig 1b:
Leukaemia cutis affecting the arms |
|
 |
Fig 1c:
Leukaemia cutis affecting the legs. |
|
 |
Fig 1d:
Close view of the leukaemia cutis lesions. |
|
A skin biopsy was taken from the chest and he was
referred to the haematologist urgently with the suspicious clinical
diagnosis of leukaemia cutis. By the time he was seen by the haematologist,
the rash started to coalesce into geographic patches covering the lower
trunk, abdomen, and proximal extremities.
Second blood film 3 months following the appearance of
the skin lesions showed 20 % circulating myeloid blasts (Fig. 2),
positive to CD33, CD117, and FLT3 phenotype. Skin
biopsy showed infiltrative sheets of atypical blastoid cells in the dermis
mainly perivascular and periadnexal (Fig. 3a, 3b) with positive
myeloperxidase staining (Fig. 4), compatible with the diagnosis of
acute myeloid leukaemia (AML) which was confirmed by the bone marrow biopsy.
 |
Fig 2:
A peripheral blood smear containing blast cells having a little
cytoplasm. |
|
 |
Fig 3a:
Atrophic epidermis, grenz zone and diffuse infiltrate of blast cells
in the dermis (H & E, X 40). |
|
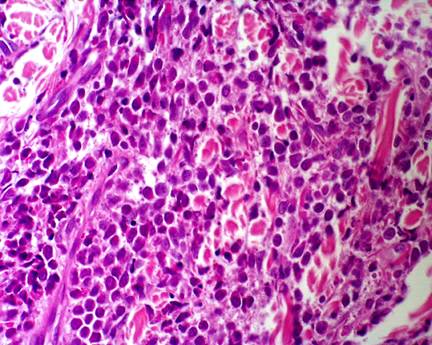 |
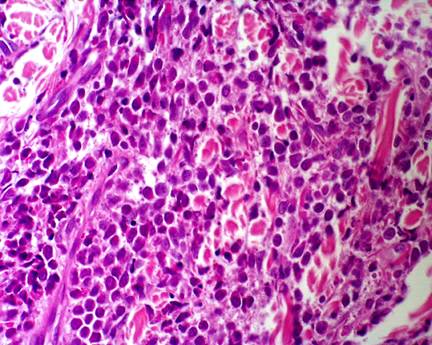
Fig 3b:
(H & E, X 100), demonstrates densely blast cells in the dermis. |
|
 |
Fig 4:
Meloperxidase(X100) staining shows positive blast cells. |
|
Discussion:
A leukaemic leukaemia cutis (ALC) is a rare condition
with a poor prognosis that has been described as skin involvement by
leukaemic cells before their appearance in the peripheral blood or bone
marrow [1].
In most cases of leukaemia cutis, systemic disease precedes the development
of skin lesions. However, in as many as less than 10% of patients with
leukaemia cutis [2],
localized skin lesions occur
prior to bone marrow infiltration and systemic symptoms (aleukemic leukaemia
cutis or primary extramedullary leukaemia).
A literature review showed that aleukaemic leukaemia
cutis confined to the skin is extremely rare and commonly misdiagnosed [3,4].
Its recognition is important because early diagnosis can lead to a better
prognosis.
As it was mentioned earlier in our case he was under
treatment with his GP for several weeks before he was seen by a
dermatologist; he was generally well with even normal investigation. There
is no clear evidence between the effects of skin infiltration on leukaemia
prognosis. However ALC is usually associated with a very poor prognosis in
leukaemic patients [3,5].
Wilkins and Janes reported a case of ALC in a 57 years
old lady who has had a fatal outcome within 11 months of the diagnosis of
skin lesions [3].
Recently Dekio et al described a case of ALC in a middle aged lady who had
passed away within 4 months of the skin rashes [6].
More recently Vishalakshi et al presented a case of ALC in a young man who
had died within 3 months of the diagnosis of the skin eruption [7].
Aleukaemic
leukaemia cutis is easily to be misdiagnosis, and has always been a
dermatological curiosity. This case has been reported to emphasize the
important of the clinical diagnosis with the combined role of dermatologist,
dermatopathologist and haematologist to achieve early correct diagnosis.
Acknowledgment
We would like to thank you Mrs Appleby, histopathology and haematology
departments at Southend on Sea hospital for
all their help.References
1. Baer M.R., Barcos M, Farrell H, et al. AML with leukemia cutis. Cancer 1989; 63: 2192- 2200.
2. Su WP. Clinical, histopathologic, and immunohistochemical correlations in leukemia cutis. Sem in Dermatol 1994; 13: 223- 230.
3. Wilkins R, Janes S. Aleukaemic leukaemia cutis: case report and review of the literature. Clin Lab Haematol 2004; 26(1): 73- 75.
4. Byrd JC, Edenfield WJ, Shields DJ, et al. Extramedullary myeloid cell tumors in acute nonlymphocytic leukemia: a clinical review. J Clin Oncol 1995; 13: 1800- 1816.
5. Paydas S, Zorludemir S. Leukaemia cutis and leukaemic vasculitis. Br J Dermatol 2000; 143: 773- 779.
6. Vishalakshi V, Torsekar R, Shinde S. Aleukemic Leukemia cutis. In J Dermatol Venereol Leprol 2007; 73: 109- 111.
7. Dekio I, Anzai H, Ohyama M, et al. Aleukaemic leukaemia cutis as an initial manifestation of myeloid/Nk cell precursor acute leukemia. JEADV 2006; 20: 453- 456.
© 2009 Egyptian Dermatology Online Journal |