|
|
Abstract:
We describe a 36 years old Chinese lady who presented with multiple
painless non- pruritc papules and nodules on the hands, elbows, ear,
face and feet associated with joint pains involving the knees and the
small joints of the hands. She also had photo- distributed rash on the
face, chest and back. Her systemic examination was normal. Other than
the articular erosions in the interphalangeal joints and erosion on the
patella bilaterally, all other investigations were normal or negative.
The photo distributed patches and plaque lesion on the front and back of
the chest with facial rash and papules on the knuckles of the hands may
be mistaken for dermatomyositis.
The histopathological examination revealed dermal infiltrates of
multinucleated histiocytic giant cells with an eosinophilic 'ground
glass' cytoplasm which confirmed the diagnosis of multicentric
reticulohitiocytosis in our case.
Introduction:
Multicentric reticulohistiocytosis (MR) is a rare disorder of skin
with systemic granulomatous involvement of no known cause with distinct
histopathology. It has been described to involve the skin, mucosa,
joints and internal organs but all the involvement may not be found in a
single patient [1]. The most prominent
clinical features are the cutaneous nodules and distinctive arthritis [2].
MR has few other names and in the literature it has been stated as
'lipoid dermatoarthritis', 'lipoid rheumatism', and 'giant cell
reticulohistiocytosis'. The confirmation of diagnosis is based on the
histological appearance of an infiltrative histiocytic multinucleated
giant cell with eosinophilic ground-glass cytoplasm [3].We
report a case of multicentric reticulohistiocytosis with skin lesions
resembling dermatomyositis probably the first reported case in Malaysia.
Case reporting:
A 36 year old Chinese lady was seen in one of our outstation
dermatology clinic in June 2007. She complained of multiple skin
coloured papules and nodules on the hands, elbows, ear, face and feet
for the last 2 years (Fig 1a- 1d). She also complained of photo
distributed erythematous patches and plaques lesion on the front and
back of the chest and some facial rash.
 | Fig 1a:
Papules, nodules on the dorsum of the hands some resembling
Gottron's papules. |
|
 | Fig 1b:
Coral beading around the finger nails. |
|
 | Fig 1c:
Cobblestone appearance papules on the elbow. |
|
 | Fig 1d:
Nodules of various sizes on the dorsum of the foot. |
|
She also complained of multiple joint pains bilaterally involving the
knees and the small joints of the hands associated with morning
stiffness for the last 6 months. She had no proximal muscle weakness.
She gave history of photosensitivity but did not complain of any
systemic problem. On examining the skin there were multiple firm papules
and nodules of different sizes ranging from few mm to 1.5 cm on the
dorsum of the hand and fingers, legs, feet, toes, both extensor aspects
of the elbows, ear and face. The papules and the nodules were painless
and non pruritic. The papules on the elbows clustered together to form a
cobblestone appearance. All routine blood and urine investigations were
normal. Her specific investigations for Rheumatoid factor, Antinuclear
antibodies, lipid profile, muscle enzymes, serum protein
electrophoresis, faecal occult blood, thyroid function tests, screening
for hepatitis B and C, HIV, VDRL, Mantoux test were found to be normal
or negative. Her cancer markers; alpha fetoprotein, CEA, Ca-125 were
normal too. Chest x-ray and abdominal ultrasound did not show any
abnormal findings. Her X-rays of the hands and knees showed articular
erosions in the interphalangeal joints and erosion on the patella
bilaterally (fig 2).
 | Fig
2: Erosions on the peripheral interphalangeal joints
bilaterally. |
|
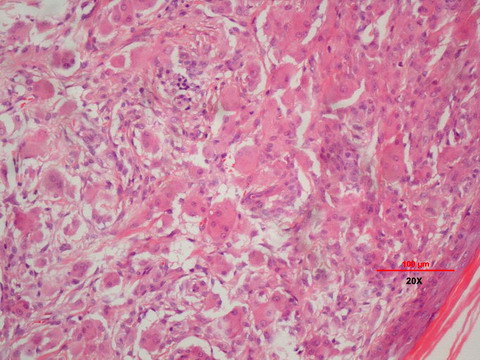
Two skin biopsies; one taken from a papular lesion on the hand and
another from a plaque lesion of the back showed similar pathology. The
HPE revealed dermal infiltrates of multinucleated histiocytic giant
cells with an eosinophilic 'ground glass' cytoplasm. Scattered
lymphocytes were seen throughout the dermis. Immuno- histochemical study
was positive for CD68 and negative for S100. These above findings
confirm the diagnosis of multicentric reticulohistiocytosis (fig 3).
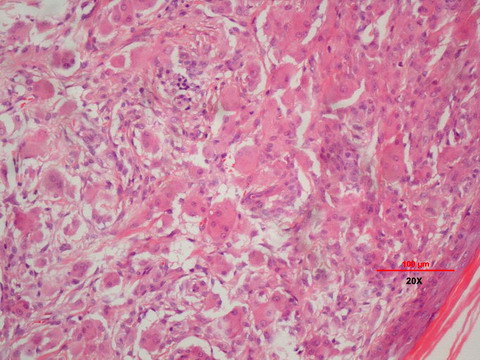 | Fig
3: Multinucleated giant cells with an eosinophilic granular
'ground glass' cytoplasm. |
|
We treated her with oral prednisolone and methotrexate initially.
Prednisolone was slowly tapered down and stopped over a 4 months period
and methotrexate was increased gradually from 5 mg to 15mg weekly and
maintained on that dose. She improved significantly during this period
.We noticed that most of the skin lesions were regressed and she
complained of less joint pain at the end of one year treatment (Fig 4-
6). Although initially we noticed some deformity of the distal interphalgeal joints of both the index fingers but during the follow-up
visits we observed that the joints were stable with no pain. At the end
of the two years in June 09, she maintained that improvement with no new
skin lesions and no worsening of joint pains and she is still maintained
on 15 mg of methotrexate weekly.
|

|

|
| Fig 4: Shows the regression of the papules and
nodules. |
|
|

|

|
| Fig 5: Shows no more cobble stone appearance on
the elbow. |
|
|

|

|
| Fig 6: Completely cleared papules and nodules on
the dorsum of the foot. |
|
Discussion:
Multicentric reticulohistiocytosis is a rare disorder with systemic
involvement for which no cause has been identified. This was first
described by Goltz and Laymon [3] in
1954 and so far only less than 200 cases have been reported. Malignancy
has been associated with MR [4]. There
is a controversy regarding its paraneoplastic nature but in about 20% of
cases it may be associated with malignancy [5].
Our patient discussed here represent with most of the cutaneous symptoms
of MR and is most likely to be the first reported case in Malaysia.
In addition to other clinical manifestations, our case presented with
erythematous papules on the knuckles of the hands (fig 1a), a patch and
like erythema on the face, plaque like eyrthema on the chest and back,
which can be mistaken for dermatomyositis but in our case the presence
of joint erosion without proximal muscle weakness and normal values of
muscle enzymes were not in favour of dermatomyositis. Moreover, skin
biopsies from two areas did not show any features of dermatomyositis but
concluded the diagnosis of multicentric reticulohistiocytosis.
Polyarthritis has been described as the commonest first presenting
symptom of MR [1,6].
We also noted similar presentation in our patient. Patient may present
only with symptoms of joint pain in about 40% of cases, only skin
lesions in 30%, and joint and skin symptom in about 30% of cases [5].
There may be other areas of involvement including the heart, lungs,
thyroid, and bone marrow [5,7].
Papules may form around the nail producing a characteristic "coral
beads" appearance as in our case (fig 1b). In about one half to one
third of cases mucosal involvement have been reported which may include
the nasal and buccal mucosa, tongue, lips larynx and trachea [1,5].
Despite extensive skin involvement, our patient did not have any mucosal
involvement. Balachandran et al [8] and
Mittal et al [6] in their reports also
did not mention any involvement of the mucosa.
There has been variable success in treating MR with corticosteroids,
hydroxychloroquine, methotrexate, alkylating agents such as chlorambucil,
cyclophosphamide, and azathioprine [9-12].
The disease activity has been reported to resolve after approximately 8
years [13]. Our patient responded
significantly with combination of oral prednisolone and methotrexate and
at the end of one year she had less joint pain and clearance of skin
lesions. Prednisolone was tapered off at four months time. As MR can
mimic dermatomyosistis, as in our case, it is important to differentiate
between the two as early treatment can prevent deformity and disability
in MR.
Acknowledgement:
Dr.Nurshaline Pauline Hj.Kipli.BDS (Dundee), FDSRCS (ENG).
We acknowledge and thank her as she helped us to obtain the
photomicrography of the HPE slide from her department.
References
1. Rao AG, Lakshmi TS, Vani V. Multicentric
reticulohistiocytosis. Indian J Dermatol Venereol Leprol 2003; 69: 35-
36
2. Karl Houlbar. Multicentric reticulohistiocytosis, in:
Fitzpatrick' Dermatology in General Medicine, 5th Edition, 1999; 183:
2095- 2098.
3. Goltz RW, Laymon CW. Multicentric
reticulohistiocytosis of the skin and synovia; reticulohistiocytoma or
ganglioneuroma. AMA Arch Derm Syphilol. Jun 1954; 69(6): 717-731.
4. Nunnink JC, Krusinski PA, Yates JW. Multicentric
reticulohistiocytosis and cancer: a case report and review of the
literature. Med Pediatr Oncol. 1985; 13(5): 273- 279.
5. Luz FB, Gaspar AP, Kalil-Gaspar N, Ramos-e-Silva M.
Multicentric reticulo-histiocytosis. J Eur Acad Dermatol Venereol. 2001;
15: 524- 531.
6. Mittel RR, Seema Gupta, Sethi PS. Case report of
atypical multicentric reticulo-histiocytosis. Indian J Dermatol Venereal
Leprol 1998; 64(3): 130- 132.
7. Rapini RP. Multicentric reticulohistiocytosis. Clin
Dermatol. 1993; 11: 107- 111.
8. Balachandran C. Sabitha C, Sandhya Acharya, et al.
Multicentri, reticulohistocytosis; Case repot. Indian J Dermatol
Venereal Leprol 1998; 64: 193- 194.
9. Cash JM, Tyree J, Recht M. Severe multicentric
reticulohistiocytosis: disease stabilization with methotrexate and
hydroxychloroquine. J Rheumatol. 1997; 24: 2250-2253.
10. Gourmelen O, Le Loet X, Fortier-Beaulieu M, et al.
Methotrexate treatment of multicentric reticulohistiocytosis. J
Rheumatol. 1991; 18: 627- 628.
11. Ginsburg WW, O'Duffy D, Morris JL, Huston KA.
Multicentric reticulohistiocytosis: response to alkylating agents in 6
patients. Ann Intern Med. 1989; 111: 384- 388.
12. Guillen C, Fortea JM, Serrano G, et al.
Multicentric reticulohistiocytosis. Dermatologica. 1984; 169: 311- 317.
13. Barow MV, Holubar K. Multicentric
reticulohistiocytosis: a review of 33 patients. Medicine (Baltimore).
1969; 48: 287- 305.© 2009 Egyptian
Dermatology Online Journal
|