Abstract:
Background: Minoxidil is a direct-acting vasodilator used for a long time to treat androgenetic alopecia as it was found to prolong the anagen phase. The mechanism of action is not fully understood. Mesotherapy is a technique which involves microinjections of conventional medication and/ or vitamins into the mesoderm or the middle layer of the skin.
Objective: to compare the effect of minoxidil as topical preparation and as mesotherapy in treatment of female pattern hair loss.
Methods: This study was conducted on 60 female patients with androgenetic alopecia and ten normal controls. Thirty patients were treated with minoxidil 2% as topical preparation and 30 were treated with intra-dermal injection of minoxidil 2% by point to point technique into deep intra-dermal of scalp using a mesogun.
Results: The results of this study revealed improvement in both self assessment evaluation and the three parameters gained by trichogram after treatment with minoxidil 2% either as topical application or mesotherapy. The use of mesotherapy showed more significant improvement than that of topical treatment.
Conclusion: this study showed that minoxidil injection by mesotherapy is more effective than using it as topical application in treatment of androgenetic alopecia in female patients. This appreciates the extension of use of minoxidil as mesotherapy. Introduction:
Androgenetic alopecia is the common type of non-scarring hair loss affecting the crown. It results from genetically determined end-organ sensitivity to androgens and is characterized by miniaturization of the hair follicles [1]. In Caucasians, it usually begins between the ages of 12 and 40 in both men and women, and affects approximately 50% of the population before the age of 50. Its prevalence was reported to be lower and its severity less among Asians, Native Americans, and African Americans [2]. It is universally accepted that dihydrotestosterone (DHT) is responsible for androgenic alopecia in men and women. DHT induces miniaturization of hair and hair follicles by accelerating the mitotic rate of the matrix, by shortening hair cycle and increasing telogen shedding, as well as by increasing the duration of the lag phase or catagen [3]. The genetics of androgenetic alopecia is complex. In general, androgenetic alopecia is believed to be due to an autosomal dominant gene with variable penetrance, but a polygenic inheritance has not been excluded. The association between hair loss and androgen receptor gene and ageing is confirmed [4]. Clinical findings of a decrease in density of the central scalp hair with sparing of the occipital region, no patches of hair loss, negative hair pull on the sides and back of the scalp and a normal appearing scalp are usually sufficient to diagnose androgenetic alopecia (female pattern) [5]. The diagnosis of androgenetic alopecia in women is much more difficult to make than in men, both because of less obvious patterns of hair loss than in men and because of the frequency with which other types of hair loss occur. In women, any complaint of diffuse or widespread hair loss should trigger consideration of androgenetic alopecia as a potential explanation [6]. The clinical presentation of androgenetic alopecia in women generally includes diffuse thinning over the fronto-parietal scalp with a preserved frontal hairline. Depending on the severity of thinning, the condition may be divided into 3 stages of hair loss as described most commonly by Ludwig's classification. In its earliest, the least severe form, thinning is minimal and would be classified as Ludwig stage I. Here androgenetic alopecia may be detected as an increased frontal part width compared to occipital part width. Stage II describes more advanced fronto-parietal thinning and stage III denotes an obvious thinning or near baldness of this area while the hairline remains intact [7]. In androgenetic alopecia the terminal hair follicle size is reduced both in length and diameter. The hair bulb moves upwards in the dermis yielding a small vellus hair follicle (secondary vellus hair). Over time the terminal scalp hair follicles undergo progressively shorter and shorter cycles involving reduced anagen growth periods. Although periods of anagen are reduced catagen and telogen time periods remain the same. The net effect is that androgenetic alopecia is characterized by a gradual increase in the number of secondary vellus hair and resting telogen hair, while the anagen hair decrease in number [8]. Androgentic alopecia must be carefully investigated due to its association with serious systemic diseases e.g. insulin resistant diabetes mellitus [9], coronary heart disease [10] and hypertension [11]. Follicular miniaturization is the main event that characterizes pattern hair loss. The transformation of large terminal hairs into miniaturized vellus-like hairs accounts for the balding process. The fact that the affected hairs, although small, are not usually lost provides hope that suitable treatment can re-grow them to a size large enough to reverse hair thinning [8]. Minoxidil is a pyrimidine derivative (2, 4-diamino-6-piperidinopyrimidine-3-oxyde) initially developed as a potent antihypertensive agent. In addition to being a direct-acting vasodilator, it was un-expectantly found to stimulate hair growth in vivo, and this side effect led to its clinical use in androgenetic alopecia. It is so far unclear why minoxidil induces hair growth. Minoxidil stimulates a time-dependent increase in 3[H]-thymidine and 35[S]-cysteine incorporation in mouse vibrissa follicles and it has been suggested that this effect is mediated via the K+ channels and that a sulphatated metabolite of minoxidil exerts this effect via minoxidil -sulfotransferase which is present in hair follicle [12]. The Mesotherapy is a technique which involves microinjections of conventional medication and/ or vitamins into the mesoderm or middle layer of the skin to promote healing or corrective treatment to a specific area of the body. Mesotherapy was invented by the Frenchman Dr. Michel Pistor in 1958 to treat conditions in rheumatology, sports, traumatology, infectious diseases, vascular diseases and mainly as a pain-relieving technique. The North American experience began when Dr. Lionel Bissoon learned the technique in France and later popularized it in America. Treatment of alopecia is considered one of the most important applications of mesotherapy in dermatology [13]. Patient and methods:
Sixty female patients with a complaint of progressive hair thinning or loss for more than 2 years, who were diagnosed clinically as androgenetic alopecia and twenty normal controls were included. Principal exclusion criteria included, postpartum alopecia and other forms of alopecia, surgical correction of scalp hair loss, topical minoxidil use within one-year, use of drugs with androgenic or anti-androgenic properties, use of finasteride or other 5-alphareductase inhibitors, or patients with precipitating factors such as thyroid disease and anemia. None of the subjects had signs or symptoms of hyper-androgenism. The clinical severity of women with androgenetic alopecia was classified according to the global grading system as proposed by Ludwig. Ten healthy women with no complaint and symptoms of hair thinning or alopecia or history of hair disease were taken as the control group. Informed consent was obtained from all subjects. Patients were randomly classified into two groups: Group (I): It was consisted of 30 patients received local applications (2 mL/ day for 12 weeks) of topical minoxidil 2%. Group (II): and 30 patients treated by minoxidil 2% injected by point to point technique, 0.1 cc every 2 cm deep intra-dermally in the scalp by mesogun
(Fig.1) (once weekly for 4 weeks then once every 2 weeks for 8 weeks).
Patients performed self-assessment of both the effect on hair growth and the effect on hair loss before and 4weeks after treatment. They assessed the effect on hair growth using the following 5-point scale: 1- Markedly improved (3 points): dense hair growth (hair growth observed over almost the entire area). 2- Moderately improved (2 points): moderate hair growth (partial hair growth easily noticeable). 3- Slightly improved (1 point): slight hair growth (hair growth slightly noticeable). 4- Unchanged (0 point): no visible hair growth. 5- Worsened (-1 point): decreased hair growth (bald area increased, with thinning hair more noticeable than at baseline). They assessed the effect on hair loss using the following 3-point scale: good (1 point): decreased hair loss; unchanged (0 point): no change in hair loss; and worsened (-1 point): increased hair loss. Summation of the points of hair growth and decrease in hair loss are obtained for both groups [3]. Both patints and controls were subjected to trichogram (Hair pluck test) before and 4 months after start of treatment. Examination was carried out at a standard time (at least 4 days) after the last washing of the hair. The examined areas were through out the scalp. The hair was cut to about 0.5cm above the scalp surface and about four to seven hairs extracted with a rapid tug by tightly closing spade-ended epilating forceps placed as close to the skin as possible. The procedure was repeated in contiguous areas to obtain a sample of not less than 50 hairs. The hairs were immediately examined under microscope. The percentage of the folowing was detected: the anagen hair, telogen hair and secondary vellus hair [14]. Statistical analysis was done using SPSS computer software. Data were expressed as mean + standard deviation. The data were analyzed by paired-samples T test. Significant differences were reported when the p value from the t-test was less than alpha (p < 0.05). Results
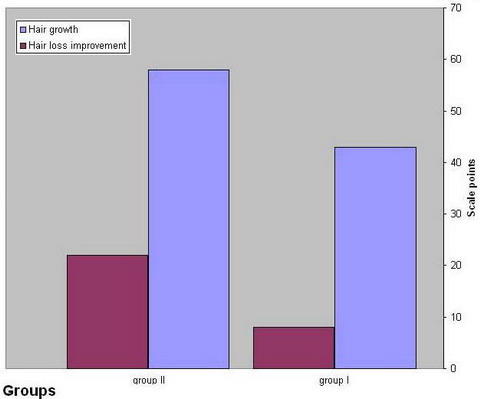
Table (1) shows the self-assessment evaluation of hair growth and hair loss improvement. The mean value of the scale points in group II was significantly higher than group I (P value < 0.05)
(Fig. 2)
|
|
|
Group I |
Group II |
|
No. |
points |
No. |
points |
|
Hair growth |
Marked |
4 |
12 |
7 |
21 |
|
assement |
Improvement |
|
|
Moderate |
6 |
12 |
9 |
18 |
|
|
Improvement |
|
|
Slight |
7 |
7 |
8 |
8 |
|
|
Improvement |
|
|
Unchanged |
11 |
0 |
5 |
0 |
|
|
Worsen |
2 |
-2 |
1 |
-1 |
|
Hair loss |
Good |
14 |
14 |
19 |
19 |
|
assement |
Improvement |
|
|
No change |
11 |
0 |
9 |
0 |
|
|
worsen |
5 |
-5 |
2 |
-2 |
|
Mean + SD |
|
|
4.75 +7.38 |
|
7.87 |
|
9.99 |
|
P value |
0.03 (< 0.05) significant |
Table 1: Self- assessment scales in patient groups
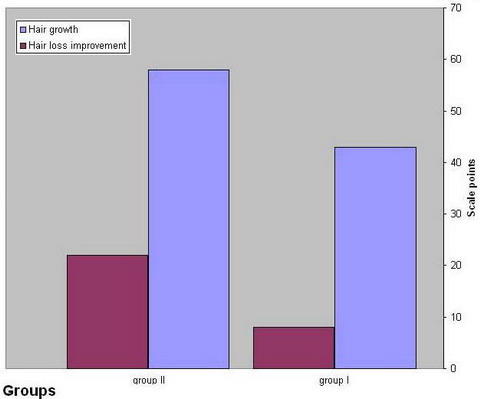 | Fig
2: Self-assessment evaluation of hair growth and hair loss
improvement. |
|
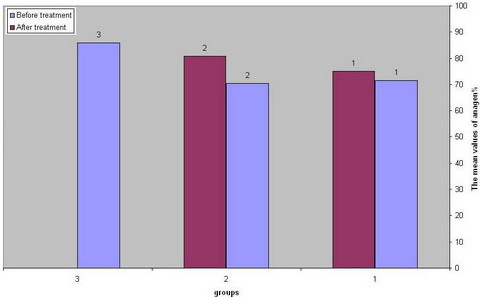
Table (2) shows the mean values +/- standard deviation of anagen hair percentage in different groups. The mean values in both groups before treatment were significantly lower than the control (P value < 0.01). There is significant increase in mean values of anagen hair percentage after treatment in both groups compared to the values before treatment (P value < 0.01). But the mean value after treatment in group II is significantly higher than that of group I (P value < 0.01).
(Fig. 3)
|
Groups |
Before treatment |
After treatment |
|
Group I |
71.53 +/- 2.79 |
75.13+/-2.84 |
|
Group II |
70.43+/- 2.46 |
80.77 +/- 2.18 |
|
Control |
85.97 +/- 1.9 |
Table 2: The mean values + standard deviation of anagen hair percentage in different groups.
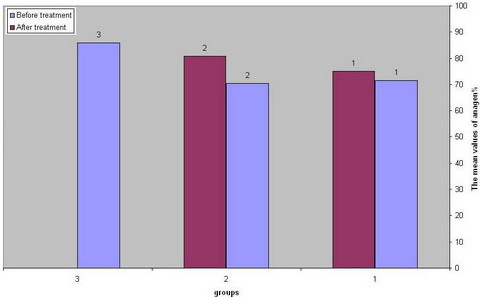 | Fig
3: The mean values of anagen hair percentage in different
groups. |
|
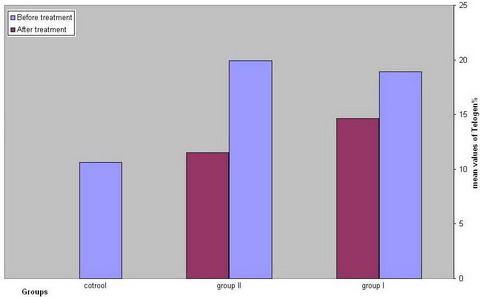
Table (3) shows the mean values + standard deviation of telogen hair percentage in different groups. The mean values in both groups before treatment were significantly higher than the control (P value < 0.01). There is significant decrease in mean values of telogen hair percentage after treatment in both groups compared to the values before treatment (P value < 0.01). But the mean value after treatment in group II is significantly lower than that of group I (P value < 0.01).
(Fig. 4)
|
Groups |
Before treatment |
After treatment |
|
Group I |
18.93 +/- 4.15 |
14.63 +/- 3.23 |
|
Group II |
19.9 +/- 3.14 |
11.5 +/-3.43 |
|
Control |
10.6 +/- 1.99 |
Table 3: The mean values +/- standard deviation of Telogen hair percentage in different groups.
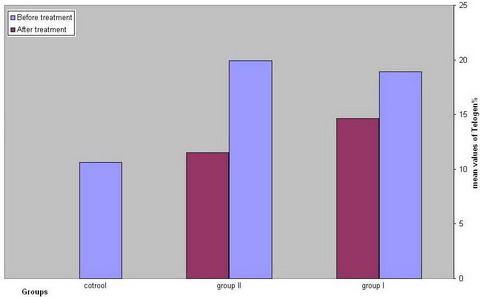 | Fig
4: The mean values of Telogen hair percentage in different
groups. |
|
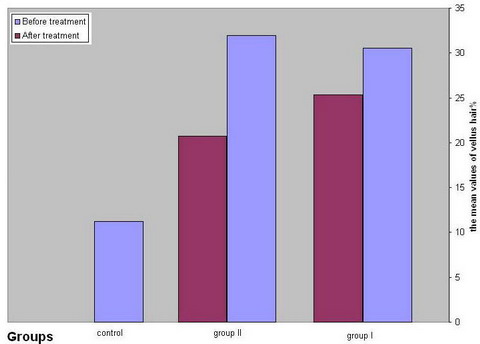
Table (4) shows the mean values + standard deviation of vellus hair percentage in different groups. The mean values in both groups before treatment were significantly higher than the control (P value < 0.01). There is significant decrease in mean values of vellus hair percentage after treatment in both groups compared to the values before treatment (P value < 0.01). But the mean value after treatment in group II is significantly lower than that of group I (P value < 0.01).
(Fig.5)
|
Groups |
Before treatment |
After treatment |
|
Group I |
30.57 + 3.39 |
25.37 + 3.39 |
|
Group II |
31.97 + 3.37 |
20.73 + 1.31 |
|
Control |
11.2 + 2.89 |
Table 4: The mean values + standard deviation of vellus hair percentage in different groups.
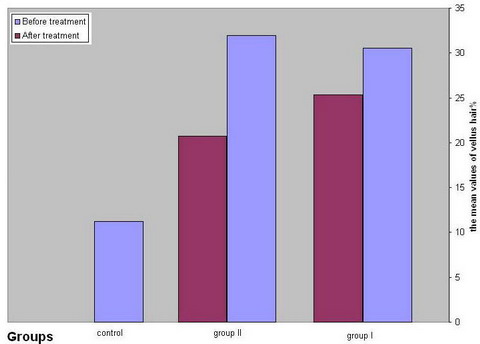 | Fig
5: The mean values of vellus hair percentage in different
groups. |
|
Figures (6) and (7) showed two patients before and after 3 months of mesotherapy treatment
|

|

|
| Fig 6: Androgenetic alopecia before (a) and after
(b) mesotherapy. |
|
|

|

|
| Fig 7: Androgenetic alopecia before (a) and after
(b) mesotherapy. |
|
Discussion:
The term androgenetic alopecia (AGA) was coined by Orentreich in 1960, but the same condition has been termed "diffuse alopecia," "female pattern alopecia," and "male pattern baldness." Orentreich's term captures a proposed cause of the alopecia, namely the genetically determined susceptibility of hair follicles to miniaturize in the presence of androgens [7]. Androgenetic alopecia (Female pattern) is characterized by a diffuse reduction in hair density which mainly affects the crown and frontal scalp with retention of the frontal hairline. Diffuse central thinning, frontal accentuation ("Christmas tree" pattern) and, although uncommon, fronto-temporal recession/vertex loss are the presenting patterns of androgenetic alopecia. In addition, bitemporal thinning is commonly associated with androgenetic alopecia. Ludwig graded androgenetic alopecia into three levels according to the severity of diffuse central thinning, while progression of hair loss according to frontal accentuation has been suggested by Olsen. Clinical findings of a decrease in density of the central scalp hair with sparing of the occipital region, no patches of hair loss, negative hair pull on the sides and back of the scalp and a normal appearing scalp are usually sufficient to diagnose FPHL, although biopsy may be required in difficult cases [15] Minoxidil (2-4diamino-6-piperidinepyrimidine-5-oxide) is a potent anti-hypertensive agent. It also makes hair grow. A pharmacologic effect that came to light as an incidental observation (side effect) has, after a decade of systematic and thorough scientific researches, become the principal usage of the drug. Enough information is now available to allow rational and optimal use of minoxidil as a hair growth promoting agent. How does minoxidil induce hair growth? It is likely not simple vasodilatation and increased vascular perfusion of the hair follicles. For it has been observed that other potent vasodilators, such as transdermal nitroglycerin, fail to stimulate hair growth. Studies to investigate the biological effects of minoxidil have revealed that it is, beside being a smooth muscle relaxer and vasodilator, a cell mitogen, an immune suppressant, and, phosphodiesterase inhibitor [16]. Minoxidil inhibits prostaglandin 1,2 formation in cultured human keratinocytes, inhibits lysyl hydroxylase in cultured human fibroblasts, and acts as K-channel agonist in human vascular smooth muscle At a cellular level minoxidil is believed to act in the region of the dermal papilla; a specific receptor site for minoxidil is being considered but is yet to be found. Histopathological changes of androgenetic alopecia include follicular miniaturisation and reduction in mean hair shaft diameter, increase in telogen germinal units, lamellar proliferation of perifollicular fibrous tissue, closed lumina of perifollicular blood vessels, and inflammatory infiltrate of variable proportions of T-cells (helper/suppressor, activated/non-activated), monocytes and Langerhans cells, only the follicular features are altered by topical minoxidil. Following topical minoxidil treatment, the hair diameter enlarges, and the anagen phase appears to become prolonged [17]. Although mesotherapy sounds like a new technique in dermatology, the scientific basis of mesotherapy is not established. It is not yet approved by the US FDA and scientific data to support its efficacy is lacking. These make a controversy about mesotherapy as a treatment modality between dermatologists. More controlled studies and standardization of the doses of the treatment materials are needed to support the use of mesotherapy on a large scale [12]. The results of this study revealed improvement in both self assessment evaluation and the three parameters gained by trichogram, the percentage of the anagen hair, telogen hair and secondary vellus hair, after treatment with minoxidil 2%. Although there was improvement with both topical application and mesotherapy but the parameters obtained by mesotherapy showed more significant improvement than that of topical treatment. There are 2 possible mechanisms to explain that, the first is that mesotherapy enabled direct inoculation of minoxidil at lower dermis near the hair follicle so more powerful action of minoxidil, the second is the multiple micro trauma obtained by mesogun needle may stimulate regenerating cytokines and growth factors to augment the action of minoxidil on the hair follicle. We concluded from this study that minoxidil injected by mesotherapy is more efficient than that of topical application in treatment of female pattern hair loss. So we recommend the extension of using mesotherapy in treatment of androgenetic alopecia in females. More researches are needed to elucidate the exact mechanism of action. References
1. Tosti A. and Piraccini B.M. Androgenetic alopecia. Int J Dermatol, 1999; 38: 1-7.
2. Tsuboi R., Tanaka T., Nishikawa T., et al. A randomized, placebo-controlled trial of 1% topical minoxidil solution in the treatment of androgenetic alopecia in Japanese women. Eur J Dermatol, 2007; 17 (1): 37- 44.
3. Olszewska M. and Rudnicka L. Effective treatment of female androgenic alopecia with dutasteride. J D D, 2005; 4: 637- 640.
4. Levy-Nissenbaum E., Bar-Natan M., Frydman M., et al. Confirmation of the association between male pattern baldness and the androgen receptor gene. Eur J Dermatol, 2005; 15: 339- 340.
5. Olsen E.A. The midline part: An important physical clue to the clinical diagnosis of androgenetic alopecia in women. J Am Acad Dermatol, 1999; 40: 106- 109.
6. Olsen A.E. Female pattern hair loss. J Am Acad Dermatol, 2001; 45:S70-80.
7. Chartier M.B.and Hoss D.M., Grant-Kels J.M. 4-Approach to the adult female patient with diffuse nonscarring alopecia. J Am Acad Dermatol, 2002; 47: 809-818.
8. Whiting D.A. Possible mechanisms of miniaturization during androgenetic alopecia or pattern hair loss. J Am Acad Dermatol, 2001; 45: S81- S86.
9. Ekmekci T.R., Ucak S, Basat O., et.al. The presence of insulin resistance and comparison of various insulin sensitivity indices in women with androgenetic alopecia. Eur J Dermatol, 2007; 17(1): 21- 25.
10. Sasmaz S, Senol M, Ozcan A, et al. The risk of coronary heart disease in mean with androgenetic alopecia. J Eur Acad Dermatol Venereol, 1999; 12: 123- 125.
11. Ahouansou S., Le Toumelin P., Crickx B., et al. Association of androgenetic alopecia and hypertension. J Eur Acad Dermatol Venereol, 2007; 17: 220- 222.
12. Hoffmann R.and Happle R. Current understanding of androgenetic alopecia. Part II: clinical aspects and treatment. Eur J Dermatol, 2000; 10 (5): 410- 417.
13. Maya V. Mesotherapy. IJDVL, 2007; 73(1): 60- 62.
14. Chamberlain A.J. and Dawber R.P. Methods of evaluating hair growth. Australas J Dermatol., 2003; 44(1): 8- 10.
15. Aktan S., Akarsu S., Ilknur T., et al. Quantification of female pattern hair loss: a study in a Turkish population. Eur J Dermatol, 2007; 17(4): 321- 324.
16. Price V.H.: Androgenetic alopecia and hair growth promotion state of the art: present and future, Clin Dermatol, 1988; 6: 218- 227.
17. Raj K. Topical minoxidil in androgenetic alopecia, how good is it? IJDVL, 1990, 56 (3): 187- 192.© 2010 Egyptian Dermatology Online Journal |