|
|
Abstract
Porokeratosis of Mibelli (PM) is a clonal disorder of keratinization.
It clinically presents with one or more annular plaques with central
atrophy and elevated keratotic borders. With a 7.5 percent risk of
malignancy, PM should be treated to prevent transformation into squamous
cell carcinoma, Bowen's disease, or basal cell carcinoma. Multiple
treatment options are available; however, there is not one universally
effective treatment. Here we describe the successful treatment of a
giant porokeratosis of Mibelli of the right lower lateral leg of a
32year-old man with topical 5 % 5-fluorouracil.cream only. After follow
up of one year, there was no development of recurrence of the lesion.
Case report
A young man of 32-years came to us with a 12 years history of a
hyperkeratotic scaly annular plaque with central atrophy on the lower
lateral aspect of the right leg (Figure 1). The lesion gradually grew to
its current size of 17/8 cm but was without itching, tenderness, pain,
redness or warmth. At the time of examination, multiple small papules
and plaques of typical porokeratosis 7- 8 in number were found in
asymmetrically on the trunk and extremities. There was no family history
of any form of porokeratosis of him.
The patient's clinical history and physical examination suggested
porokeratosis of Mibelli. A punch biopsy of the plaque was performed.
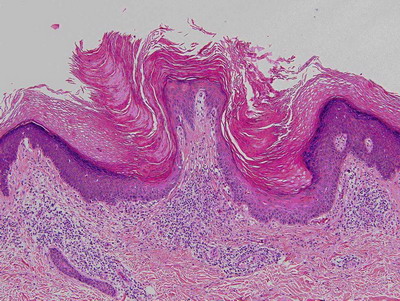
Histopathologic examination demonstrated a mildly acanthotic epidermis
with columns of parakeratosis overlying dyskeratotic keratinocytes with
absence of an intervening granular layer. A lichenoid lymphocytic
infiltrate was seen in the superficial papillary dermis (Figure 2) . The
histopathologic findings were consistent with porokeratosis.
The giant plaque porokeratosis on his right ankle was initially
treated with topical steroid and cryotherapy but the improvement was not
rewarding. The plaque became susceptible to develop infection for which
the patient often had to take antibiotic. We decided to treat the
patient with topical 5 percent 5-fluorouracil every morning and night
for 8 weeks. On follow-up, the annular plaque on the patient's right
ankle appeared erythematous and irritated. The patient continued the
treatment for 4 additional weeks. On examination, the treated area
appeared well healed with mild residual hyper pigmentation after a total
period of 12 weeks (Figure 3). All other plaques of porokeratosis healed
earlier than the giant form of PM.
 |
Fig1. Hyperkeratotic scaly annular plaque with central atrophy on the
right leg. |
|
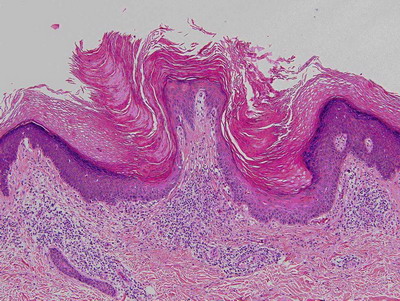 |
Fig2. H & E section from skin biopsy showing: acanthotic epidermis,
columns of parakeratosis overlying dyskeratotic keratinocytes , absence
of an intervening granular layer and lichenoid lymphocytic infiltrate in
the superficial papillary dermis |
|
 |
Fig3. Porokeratosis after treatment |
|
Discussion
Porokeratosis is heterogeneous group of disorders that are inherited
in an autosomal -dominant fashion[1].
Usually it is presented as 1 or more atrophic plaques bordered by a
hyperkeratotic ridge-like border. There are five clinical variants of
porokeratosis: classic porokeratosis of Mibelli, disseminated
superficial actinic porokeratosis, porokeratosis palmaris et plantaris
disseminata, linear porokeratosis, and punctate porokeratosis [2].
Our patient presented with a giant PM.
Classic porokeratosis of Mibelli begins during infancy or childhood
as asymptomatic small brown to skin colored papules and plaques with a
characteristic annular border [3] .
Porokeratosis of Mibelli classically presents with one or multiple
annular plaques with central atrophy and elevated keratotic borders that
have a longitudinal furrow [2].The
well-demarcated hyperkeratotic border is usually more than 1 mm in
height, with a characteristic longitudinal furrow. The center of the
lesion may be hyperpigmented, hypopigmented, depressed, atrophic or
anhydrotic.[3].Lesions range in diameter
from millimeter to several centimeters, but giant lesions measuring up
to 20 cm may occur. Such giant porokeratosis are rare and occurs
predominantly on the lower leg and foot. Porokeratosis has also been
known to occur on the face, palms and soles, genitalia, and buccal
mucosa [4]. If the nail matrix is
involved ,nail dystrophy may develop. Lesion may appear during the
chemotherapy for malignancy, after the renal transplantation.[1]
Histopathologically, PM has the cornoid lamella, a column of
parakeratosis arising within the invagination of the epidermis. The
granular layer is focally diminished and keratinocytes are dyskeratotic
[5].
Porokeratosis of Mibelli has been associated with an increased risk
of malignant transformation into squamous-cell carcinoma and Bowen
disease, as well as basal-cell carcinoma [4],
with rates as high as 7.5 percent. Large lesions are of a higher
malignant potential.[12] As a result,
treatment is necessary when PM is diagnosed. Potential therapies include
topical 5-fluorouracil, CO2 laser ablation, 585-nm pulsed dye laser
radiation, oral retinoids, Grenz ray radiation, Nd:YAG laser radiation,
cryotherapy, dermabrasion, surgical excision, electrodesiccation, and
imiquimod [11].
A fluorinated pyrimidine, 5-fluorouracil, disrupts DNA synthesis by
disrupting thymidine synthesis. This leads to cytotoxic activity towards
rapidly dividing cells in the S phase. Because of the hyperproliferative
nature of porokeratosis, topical 5-fluorouracil produces an inflammatory
response [6]. Both topical as well as
systemic 5-fluorouracil has been shown to be efficacious in the
treatment of porokeratosis [6,7].
Multiple published case reports of PM treated with 5 percent topical
imiquimod have documented its efficacy [8,9,10].
Occlusion of the lesion was an important factor leading to resolution of
the lesion.
This report describes a patient with PM on the right ankle treated
with topical 5 percent 5-fluorouracil, that induced complete resolution.
We conclude that treatment with topical 5 percent 5-fluorouracil is
another therapeutic option for PM. Further investigation of the
efficacy, tolerability, and side effects of 5-fluorouracil in PM is
needed.
References
1. William DJ,Timothy GB, Dirk ME; Andrew's diseases of
the skin Clinical Dermatology 2006,10th edi., p-566
2. Pizzichetta MA, Canzonieri V, Massone C, Soyer HP.
Clinical and dermoscopic features of porokeratosis of Mibelli. Arch
Dermatol. 2009;145:91-92.
3. Lin J-H, Hsu MM-L, Sheu H-M, Lee JY-Y. Coexistence of
three variants of porokeratosis with multiple squamous cell carcinomas
arising from lesions of giant hyperkeratotic porokeratosis. J Eur Acad
Dermatol Venereol. 2006;20:621-623.
4. Kanitakis J, Euvrard S, Faure M, Claudy A.
Porokeratosis and immunosuppression. Eur J Dermatol. 1998;8:459-465.
5. Alexis AF, Busam K, Myskowski PL. Porokeratosis of
Mibelli following bone marrow transplantation. Int J Dermatol.
2006;45:361-365.
6. Nahm WK, Donohue KG, Danahy JF, Badiavas E, Falanga
V. Systemic 5-fluorouracil producing an inflammatory response in
porokeratosis. J Eur Acad Dermatol Venereol. 2003;17:190-192.
7. McDonald SG, Peterka ES. Porokeratosis (Mibelli):
treatment with topical 5-fluorouracil. J Am Acad Dermatol.
1983;8:107-110.
8. Jain S. Successful treatment of porokeratosis of
Mibelli with imiquimod 5% cream. Clin Exp Dermatol. 2006;31:302-303.
9. Harrison S, Sinclair R. Porokeratosis of Mibelli:
successful treatment with topical 5% imiquimod cream. Australas J
Dermatol. 2003;44:281-283.
10. Agarwal S, Berth-Jones J. Porokeratosis of Mibelli:
successful treatment with 5% imiquimod cream. Br J Dermatol.
2002;146:338-339.
11. Montes-De-Oca-Sanchez G, Tirado-Sanchez A,
Garcia-Ramirez V. Porokeratosis of Mibelli of the axillae: treatment
with topical imiquimod. J Dermatolog Treat. 2006;17:319-320.
12. Maubec E, Duvillard P, Margulis A, et al. Common
skin cancers in porokeratosis. Br J Dermatol. 2005;152:1389-1391.© 2011 Egyptian Dermatology Online
Journal
|