|
|
Abstract
A 35 year old married female presented with asymptomatic swellings
over lateral aspect of right foot since 1 year with occasional pain
gradually increasing in size. There was no history of any other
complaint. Rest of cutaneous and systemic examination including eye
examination was within normal limits. Biopsy from one of the lesion was
pathognomonic of erythema elevatum diutinum(EED). The patient was
treated with oral dapsone with good response within 6 months.
Key words: Unilateral, erythema elevatum diutinum, dapsone
Introduction
Erythema elevatum diutinum (EED) is a rare, form of cutaneous
leukocytoclastic vasculitis, characterized clinically by
red-to-yellow-brown papules, nodules, and plaques, typically affecting
extensor surfaces and the dorsal aspects of joints in a symmetric
distribution.[1] EED may be associated
with several immunological and infectious diseases, collagen vascular
diseases, hematological disorders, inflammatory bowel disease, B-Cell
lymphomas, Myeloproliferative disorders.[2]
Unilateral EED is a rare occurrence.
We report a case of isolated and unilateral EED treated successfully
with oral dapsone therapy.
Case report
A 35-year-old female presented with history of asymptomatic brownish
raised lesions over the lateral aspect of right foot of one year
duration. There was history of gradual increase in the number and the
size of the lesions. The lesions were not associated with itching and
burning sensation or pain. There was no history of preceding or
associated upper respiratory tract infection, gastro-intestinal
disturbances, fever and malaise. She was not a known diabetic or
hypertensive and had no past history of tuberculosis or contact with
tuberculosis.
On examination her vital parameters were within normal limits. There
were multiple unilateral brownish nodules on the lateral aspect of right
foot (Fig 1). No similar lesions were seen anywhere else. The
nodules were brownish, smooth surfaced, firm in consistency, non-tender
and not fixed to the underlying tissues. There was no significant
lymphadenopathy, hepatosplenomegaly or joint deformity or any eye
complaint.
 | Fig 1:
Multiple brownish nodules over right lateral foot. |
|
The differential diagnosis of Keloid, fibromatosis and late stage
Kaposi's sarcoma were thought and patient was investigated.
The complete hemogram, blood biochemistry, X-ray chest and
electrocardiogram were normal. ASLO titer was normal and throat swab did
not show any growth. The tests for rheumatoid factor, ANA, dsDNA as well
ELISA for HIV were negative. Serum IgA, IgG and IgM levels were within
normal limits. Urine examination for Bence-Jones proteins was negative.
Eye examination revealed no abnormality.
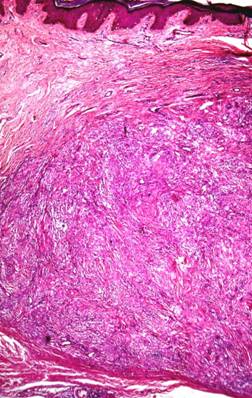
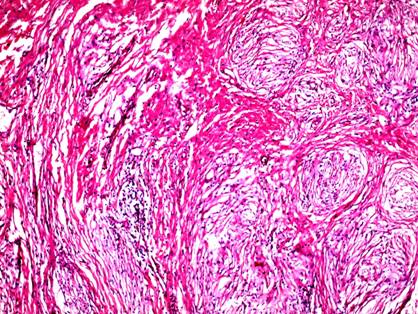
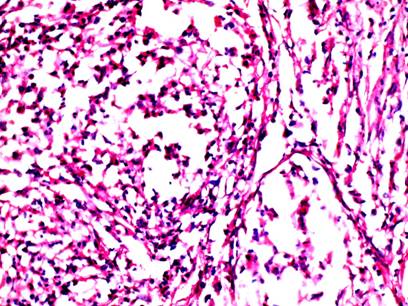
Skin biopsy from a nodule revealed normal epidermis and a
circumscribed dense dermal infiltrate of predominant neutrophils with
few lymphocytes, eosinophils especially in the perivascular areas with
fibroplasia and thickening of collagen (Fig 2,3). The blood
vessels showed endothelial cell swelling, infiltration of walls with
neutrophils, extravasation of erythrocytes and perivascular nuclear dust
and perivascular fibrosis (Fig 4).
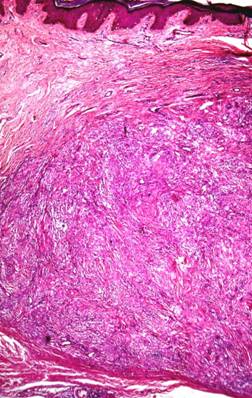 | Fig
2: A circumscribed collection of inflammatory infiltrate in
dermis with fibroplasia. (H&E, 25X). |
|
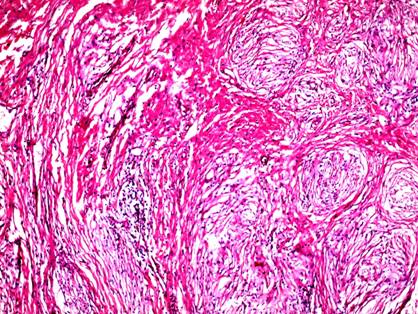 | Fig
3: Dense mixed infiltrate with predominance of neutrophils,
nuclear dust, perivascular fibrosis and vessel damage. (H&E,
100X) |
|
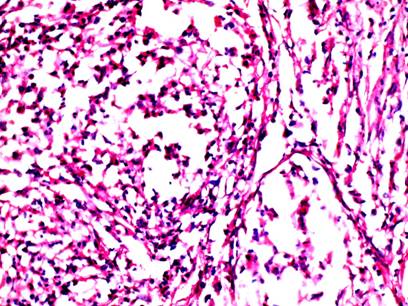 | Fig
4: The infiltrate invading vessels shows neutrophils with
nuclear dust. (H&E, 400X). |
|
On clinico-pathological correlation the final diagnosis of unilateral
isolated erythema elevatum diutinum (EED) was made. The patient was
started on 100 mg of dapsone daily at bed time. A significant flattening
of the lesions was noticed by the end of six months of therapy
(Fig 5).
 | Fig
5: Nearly complete flattening of lesions after 6
months of dapsone therapy. |
|
Discussion
It was first described by Hutchinson in 1888 and by Bury in 1889. [2]
It is a rare form of cutaneous leukocytoclastic vasculitis,
characterized clinically by red-to-yellow-brown papules, nodules, and
plaques which typically occur over extensor surfaces and the dorsal
aspects of joints in a symmetric distribution. The trunk and the mucosae
are usually spared. Rare presentations include vesicular, bullous, and
ulcerative lesions. Lesions are generally asymptomatic but occasionally
may be tender, painful, or pruritic. Constitutional symptoms like
arthralgias and fever may occur though systemic vasculitis is not
present. It occurs usually in third to sixth decade but childhood cases
especially with vesiculo-bullous lesions also occur. The disease follows
chronic course with frequent relapses although it may spontaneously
remission may occur rarely. Lesions tend to become firm and indurated
over time and heal with pigmentary changes and atrophic changes with
loss of collagen in the dermis. [1,2,3]
Exact pathogenesis of EED is not known but it is thought to be a
consequence of an arthus like reaction to bacterial or viral antigen
with formation of circulating antigen antibody immune complexes that get
deposited in dermal vessels leading to activation of complement cascade
and neutrophil activation with consequent vascular damage. [2,4,5]
EED is well known for its systemic associations like HIV infection,
chronic/recurrent streptococcal infection, verrucous cutaneous
carcinoma, immunologic disorders, collgen vascular diseases like
rheumatoid arthritis and lupus erythematosus, hematological diseases
like IgA monoclonal gammopathy, myeloproliferative disorders,
inflammatory bowel disease, gout, scleritis and uveitis and a thorough
examination and work up of such cases is warranted to find any systemic
problem. [1,2,4,6]
It needs to be differentiated from similar conditions like granuloma
faciale, granuloma annulare, reticulohistiocytosis, xanthomas, Kaposi's
sarcoma, pyoderma gangrenosum, dermatitis herpetiformis, Sclerosing
hemangioma and dermatofibroma. Histopathology is helpful to rule out
many of these conditions.[1,2]
Histologically early lesions show a dense, perivascular, predominantly
neutrophilic infiltrate involving superficial and mid dermis with
leukocytoclasis, fibrin deposition and vascular injury though
eosinophils, plasma cells and histiocytes may be seen. Older lesions
show perivascular fibrosis with onion-peel appearance, intracellular
cholesterol deposition and capillary proliferation. [1]
Thus skin biopsy is usually diagnostic and other investigations like
direct immunofluorescence and electron microscopy may be done in
doubtful cases. [2]
Dapsone is the treatment of choice with good therapeutic response as
was seen in our case. Various other drugs like colchicine, sulfapyridine,
niacinamide and tetracycline and steroids either topical, Intralesional
or oral have been used with variable success. Most important part of
treatment is to unmask any serious systemic disease. Patients with IgA
gammopathy may need intermittent plasma exchange in addition to above
measures.
Our case showed good response to oral dapsone had no any systemic
association and lesions were unilateral, which is rare in EED.
References
1. Farley-Loftus R, Dadlani C, Wang N, et al. Erythema
elevatum diutinum. Dermatol Online J. 2008;14:13.
2. Sachdev DS, Kharkar VD, Mahajan SA, Gupte PD.
Erythema elevatum diutinum. J Postgrad Med. 2002;48:310-311.
3. Nair SR, Viswanath V, Sonavane AD, et al. Erythema
elevatum diutinum with verrucous carcinoma: a rare association. Indian J
Dermatol Venereol Leprol. 2010;76:420-422.
4. Tomasini C, Seia Z, Dapavo P, et al. Infantile
erythema elevatum diutinum: report of a vesiculo-bullous case. Eur J
Dermatol. 2006;16:683-686.
5. Gibson LE, el-Azhary RA. Erythema elevatum diutinum.
Clin Dermatol. 2000;18:295- 299.
6. Futei Y, Konohana I. A case of erythema elevatum
diutinum associated with B-cell lymphoma: a rare distribution involving
palms, soles and nails. Br J Dermatol. 2000;142:116-119.
© 2011 Egyptian Dermatology Online Journal
|