|
|
Abstract
Xeroderma pigmentosum is a rare autosomal recessive disorder characterized
by photosensitivity, pigmentary changes, premature skin aging and malignant
tumour development due to cellular hypersensitivity to ultraviolet radiation
resulting from a defect in DNA repair. A 47 years old female presented with
an increase in size and ulceration of the pre-existing pigmented macules over
the face. The patient had these hyperpigmented macules since early childhood,
throughout the body, more on sun exposed areas. Histological examination of
ulcero-proliferative lesions showed features of malignant melanoma while the
surrounding hyperpigmented macules revealed changes of xeroderma pigmentosum.
This case highlights a rare clinical entity presenting with a complication
which is even rarer.
Introduction
Xeroderma pigmentosum is a rare autosomal recessive disorder. [1] It is seen in all races worldwide and has equal sex
incidence. It occurs with an estimated frequency of 1: 250,000 in United
states and is somehow more common in Japan, but its incidence is not significant
in India. [2,3,4] It is characterized by photosensitivity,
pigmentary changes, premature skin aging and malignant tumour development
which commonly include squamous cell carcinoma, basal cell carcinoma and
rarely fibrosarcoma. Malignant melanoma arises in only about 3% of patients
with xeroderma pigmentosum. The basic defect underlying the clinical
manifestation is a nucleotide excision repair (NER) defect leading to
defective repair of DNA damaged by UV radiation.[3]
Here is a case report of malignant melanoma arising in a patient of
xeroderma pigmentosum.
Case Report
A 47 years old female reported with chief complaints of freckles and
hyperpigmented macules all over the body as well as photo-sensitivity and
increased watering from eyes since early childhood. These skin lesions
initially appeared over the face and gradually involved the entire body
surface. The skin pigmentation was progressive and more so after exposure to
sunlight. She presented with increase in size and ulceration of two lesions
over the face since one month. There was no history of consanguinity and the
parents and the other siblings were normal.
|

|
Fig
1: Segmental
vitiligo lesions: lesions affect different body sites
|
|
Fig.1: Multiple pigmented ulcero-proliferative lesions on the face.
Local examination revealed pigmented ulcero-proliferative lesions over the
face varying in size from 1 to 1.5cm with crusting and hemorrhage. Multiple
pigmented macules and freckles were noticed over the rest of the body.
Lesions were more over the sun exposed areas. There was no significant
cervical lymphadenopathy. Systemic examination was essentially normal.
Complete haemogram and serum biochemistry was within normal limits. Chest
radiography and ultrasonography of the abdomen were normal.
|
|
|
|
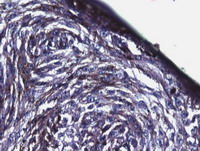
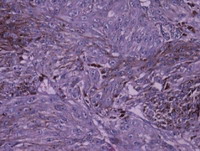
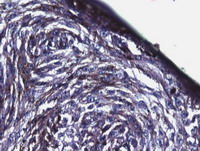
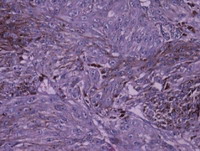
Fig
2, 3: Photomicrograph
of biopsy of pigmented lesions showing pleomorphic tumour cells with
melanin pigment. [H,EX2OO]
|
|
Wedge biopsy of ulcerated skin lesion over the face revealed tumour cells
containing melanin pigment. High power view revealed pleomorphic cells with
moderate amount of cytoplasm, vesicular nuclei, prominent nucleoli and
melanin pigment.
|
|
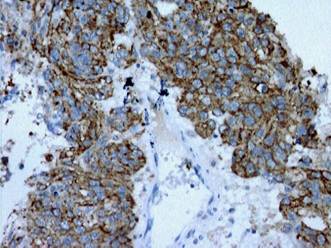
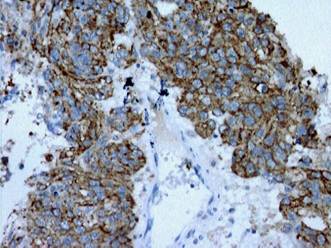
Fig
4: Photomicrograph
showing HMB 45 positivity in tumour cells on immuno-histochemistry.
[IHCX200]
|
|
On immuno-histochemistry, the tumour cells were positive for HMB-45 and
S-100. The histological features were consistent with those of malignant
melanoma.
|

|
Fig
5: Photomicrograph
of biopsy from macules showing features of Xeroderma Pigmentosum.
[H,EX200]
|
|
Biopsy from hyperpigmented macular lesions over the body showed features
consistent with Xeroderma pigmentosum.
The patient was offered conservative treatment with antibiotics and wound
care and was referred to plastic surgery where she underwent excision of both
lesions.
Discussion
Xeroderma pigmentosum is a rare autosomal recessive disorder. It was first
described in 1874 by Hebra and Kaposi. In 1882, Kaposi coined the term
Xeroderma pigmentosum. [1,2] It has been reported worldwide in all races with an
estimated frequency of 1: 250,000 in US and somehow is more common in Japan.[2,3,4] In these patients excessive solar damage to the skin
develops at an early age. The lesions occur chiefly in areas of skin that
habitually are exposed to sunlight. Three stages are recognized; the first
stage usually starts when the child is 1-2 years old, there occurs slight
diffuse erythema which is associated with scaling and small areas of
hyper-pigmentation resembling freckles. In the second stage, atrophy of the
skin, mottled pigmentation and telangiectasias develops which give the skin
an appearance similar to that of a chronic radio-dermatitis. Third stage
usually starts in adolescence; various types of malignant tumors of skin
appear, often causing death. Malignancies include squamous cell carcinoma,
basal cell carcinoma and rarely fibrosarcoma. Only about 3% of patients
develop malignant melanoma. The eyes are commonly affected showing
conjunctivitis and often keratitis with corneal opacities. [1] Apart from occulo-cutaneous malignancies very rarely it
may be associated with neoplasm of other organs like brain, bone marrow,
stomach, testis, lungs, pancreas etc.[6]
The basic defect in xeroderma pigmentosum is in the nucleotide excision
repair (NER) leading to deficient repair of DNA damaged by UV radiation.
There are ten genetic complementation groups, while one group exhibits
defective, post replication repair (XP variant), nine are deficient in
excision repair (XP group A-I). Owing to impaired ability to repair,
defective or damaged DNA leads to heritable chromosomal mutation and cell
death, which possibly cause neoplastic and atrophic clinical abnormalities.[7] Seven XP repair genes, XPA through XPG have
been identified. In addition to the defects in repair genes, UVB radiation
also has immuno-suppressive effects that may be involved in the pathogenesis
of xeroderma pigmentosum.[1,3] The prognosis of this disease is poor with fewer than
40% of patients surviving beyond the age of 20. Individuals with milder forms
of disease may however survive beyond middle age. [3]
Although Xeroderma pigmentosum is ultimately fatal, life can be prolonged
by paying strict attention to simple preventive measures to minimize sun
exposure. The patient should undergo regular checkups for early detection and
treatment of any malignancies that may occur to reduce the mortality [3]
References
1. Johnson BL, Yan AC, Congenital diseases (genodermatoses) in
Lever's Histopathology of the skin ed. E Elder D, Elenitsas R, Johnson BL,
Murphy GF, XU X, Philadelphia, Lippincott Williams & Wilkins,2009: 141.
2. Rao TN, Bhagyalaxmi A, Ahmed K et al, A case of melanoma in
xeroderma pigmentosum, Indian J Pathol Microbiol 2009; 52: 524- 26.
3. Pradhan E, Padhye SB, Malla OK, Karki KJD, Case of xeroderma
pigmentosum with well differentiated squamous cell carcinoma in the eye,
Kathmandu Univ Med J 2003; 4: 278- 83.
4. Mohanty P, Mohanty l, Devi BP, Multiple cutaneous
malignancies in xeroderma pigmentosum, Indian J Dermatol Venereol Leprol
2001; 67: 96- 97.
5. Patil MR, Vishwanath V, Arya M et al. Pilomatricoma in a
case of familial xeroderma pigmentosum. Indian J Dermatol Venereol Leprol
2007; 73: 198- 99.
6. Ramachandra I, Shenoi KR, Santosh Pai U, Xeroderma
pigmentosa in siblings: Cystosarcoma phylloides in a case of xeroderma
pigmentosa, Indian J Dermatol Venereol Leprol 2002; 68: 168- 70.
7. Pathy S, Naik KK, Bhasker S, Squamous cell carcinoma of face
with xeroderma pigmentosa-A case report, Indian J Med Ped Oncol 2005; 26: 47-
9. [PDF]
©
2011 Egyptian Dermatology Online Journal
|