|
|
Abstract
Pityriasis rosea (PR) is an acute, self-limited papulosquamous dermatosis
localized on the trunk and extremities, that affects otherwise healthy adolescents
and young adults. Although the classic presentation is readily recognized,
atypical forms may present a challenge. Many atypical forms of the disease
have been reported in the literature.[1]We
report two cases with atypical features. Involvement of nail folds and web
spaces of hands was seen in one case while vesicles on the erythematous
base were seen in other.
Key words: Pityriasis rosea, atypical, vesicular, nail folds exfoliation
Introduction
Pityriasis rosea (PR), first named as such by Gibert in 1860, is a fairly
common dermatosis. In its classic form, the initial lesion, also called
the herald patch, is larger than the subsequent lesions. Days to weeks later
crops of smaller macules, papules, and plaques begin to appear. Multiple
oval scaly pink lesions with typical collarette of scales, are distributed
in the so-called "Christmas tree" pattern following skin cleavage lines
on the trunk.[2]When all these features
are present, diagnosis is easiest to establish. However, atypical variants
and unusual presentations can be more challenging to diagnose and requires
a more astute observer.[1,3]
Two cases of PR, with atypical presentations are being described in this
report.
Case report
Case one
A 30-year-old man presented with multiple asymptomatic red raised scaly
lesions, mainly on upper extremities and few on abdomen since last 1 week.
There was no history of any preceding coryzal symptoms, herald patch, unprotected
sexual exposure, vaccination, drug intake or photosensitivity. Examination
revealed discrete erythematous scaly patches of variable size on arms, forearms,
proximal nail folds, palms and web spaces of bilateral hands. On closer
examination, the rash showed peripheral collarette scaling over arms and
forearms. (Fig1) The face, scalp, trunk, soles and mucous membranes
including genitalia were uninvolved.
 | Fig 1:
(a) closer view of lesions on arm showing typical collarette
scales, (b) Erythematous scaly plaques with exfoliation on
proximal nail folds and web spaces of left hand and (c)
involvement of palm |
|
Based on above findings, a diagnosis of secondary syphilis, atypical
PR and pityriasis lichenoides chronica were thought.
His complete blood picture, liver function tests and clotting profile
were normal. VDRL, HIV antibodies and antinuclear antibodies were negative.
Potassium hydroxide mount of scraping from scales revealed no fungi.
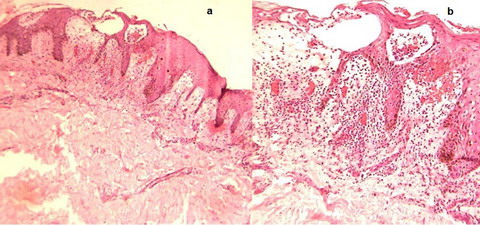
Biopsy from representative lesion showed focal parakeratosis, mild epidermal
hyperplasia and spongiotic vesicles in epidermis containing lymphoytes,
papillary dermal edema, extravasation of RBCs around superficial vascular
plexus along with moderately dense perivascular lymphocytic infiltrate.
(Fig 2) Based on clinicopathological correlation, a diagnosis of atypical
PR with nail fold, web space and palm involvement was made.
 | Fig
2: (a) Low power view showing epidermal hyperplasia with
superficial perivascular infiltrate (H&E, 40X) (b) Perivascular
lymphocytic infiltrate with extravasation of RBCs, spongiotic
vesicle in epidermis containing lymphocytes. (H&E, 100X) |
|
Patient was given oral erythromycin 2gm per day in four divided doses
for 7 days along with topical mid potent steroid cream and moisturizers.
Lesions did not increase and patient reported improvement after 2 weeks.
Lesions cleared completely over 4 weeks.
Case two
A 28- year old unmarried male presented with multiple asymptomatic red
raised and fluid filed lesions on his abdomen and lower back since 3 days.
Recently he noted that lesions are increasing in number and new lesions
are coming on upper extremities. There was no history of any preceding coryzal
symptoms, herald patch, unprotected sexual exposure, vaccination, drug intake
or photosensitivity.
Examination revealed multiple discrete erythematous, edematous papules
and vesicles on erythematous base, involving mainly abdomen, lower back
and few on upper extremties. Size of vesicles was variable with largest
being up to 0.2- 0.5cm in diameter. No scaly plaques were seen. On closer
examination, there was tiny crust at the top of some vesicles. (Fig 3)
Vesicles were distributed along the lines of cleavage. The face, scalp,
lower extremities, palms, soles and mucous membranes including genitalia
were uninvolved. He denied application of any irritant application locally.
There was no evidence of any other skin infection on his body.
 | Fig
3: (a) Multiple edematous papules and vesicles over abdomen
(b) Similar lesions on lower back (c) Closer view of abdominal
lesions showing multiple vesicles of variable size. (d) Closer
view of lesions on back |
|
Based on above findings, a diagnosis of Id eruption, vesicular PR and
irritant contact dermatitis were thought.
His complete blood picture, liver function tests and clotting profile
were normal. VDRL, HIV antibodies and antinuclear antibodies were negative.
His routine stool and urine examination with microscopy revealed no abnormality.
Biopsy from one of the vesicle was done. It showed focal parakeratosis,
moderate epidermal hyperplasia, large intraepidermal spongiotic vesicles
with exocytosis of lymphocytes papillary dermal edema, extra-vasation of
RBCs around superficial vascular plexus along with moderately dense perivascular
lymphocytic infiltrate. (Fig 4) Based on clinicopathological correlation,
a diagnosis of vesicular PR was made.
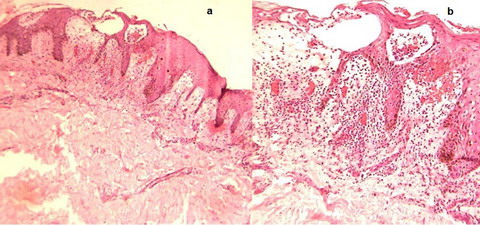 Fig
4: (a) Scanner view showing epidermal hyperplasia,
intraepidermal spongiotic vesicles, papillary dermal edema and
dense perivascular infiltrate (H&E, 40X)
(b) Subcorneal and intraepidermal spongiotic vesicles containing
lymphocytes, RBCs, congested vessels with extravasation of RBCs
and dense perivascular lymphocytic infiltrate around superficial
vascular plexus. (H&E, 100X) |
|
Patient was given oral erythromycin 2gm per day in four divided doses
for 7 days, single triamcinolone acetate 40mg intramuscular injection along
with topical mid potent steroid cream and calamine lotion. Lesions did not
increase in number and patient reported improvement over 3 weeks with nearly
complete clearence.
Discussion
Pityriasis rosea is an inflammatory skin disease characterized by erythematous
papulosquamous eruptions localized on the trunk and extremities. The eruptions
are self-limiting and usually disappear gradually in 2-10 weeks without
any treatment. Although no etiology has been proven, viral agents especially
human herpes virus 6 and 7, autoimmunity, many drugs and psychogenic status
have been proposed as possible etiological factors.[1,4,5]
Though diagnosis of PR is straight forward in its classic form, atypical
cases may be missed easily and misdiagnosed.[1]
Atypical variants of PR are rare, constituting approximately 20 percent
of all cases. [6]Atypical types can be differentiated
by size (PR gigantea of Darier, Papular PR), distribution (Cephalic PR,
inverse PR, unilateralis PR, localized PR and pityriasis circinada et marginata
of Vidal), sites involved(face, scalp, hands and feet fingers, toe tips,
eyelids, penis and oral cavity ), severity (PR irritata with severe itch,
pain and a burning sensation), course of the lesions ( like relapse, recurrent
PR , annual relapse) and morphology. [1,3,4,7]
According to morphology, atypical forms of PR are described which includes,
generalized papular, vesicular, purpuric (hemorrhagic), urticarial, pustular
and erythema multiforme like PR. Additionally, drug-induced PR-like eruptions
have been reported as separate clinical entity. [3,4]
In first case described here, atypical features included lack of involvement
of back and Christmas tree pattern, involvement of palms along with web
spaces and proximal nail folds of bilateral hand fingers with exfoliation
along with typical papulosquamous plaques with collarette scales. (Figure-1)
We could not find report of nail fold exfoliation in PR with involvement
of web spaces in literature.
In second case, atypical features includes, vesicular lesions on erythematous
base with variable size from 2mm to 5mm without typical papulosquamous eruption
of typical PR, and lack of herald patch.
Only a few vesicular PR cases have been reported in the literature and
it is seen more frequently in children and young adults. The vesicular lesions
may settle on the palms, soles, face or anterior forearm resembling varicella
or dishydrosis.[3,4,8]
No palmar lesions were seen in our case. The vesicles are usually associated
with typical papulosquamous eruptions [3,9]
. In our case there were only vesicles. Good response to erythromycin treatment
as shown by Miranda et al. and in our second case, may be due to anti-inflammatory
and immunomodulary proprieties attributed to erythromycin or antibacterial
action against Streptococcus, Chlamydia, Legionella and Mycoplama which
are thought to be etiological agents for upper respiratory tract infection,
which can be a cause of PR as per previous literature. [3,10,11]
The diagnosis was based on clinical appearance of the lesions and histopathological
findings in both the cases. There was no suggestion of herald patch in both
the cases. In both the cases lesions subsided over a period of 6-8 weeks
and patients are free of symptoms as per communication. There was no residual
pigmentary change or scarring noted in both cases and no recurrence is seen
till now.
Atypical cases of pityriasis rosea (PR) are fairly common and less readily
recognized. Physicians should be aware of the wide spectrum of PR variants
so that appropriate management and reassurance can be offered. Two cases
described here would help to increase recognition of PR.
References
1. Chuh, A., Zawar, V. and Lee, A. Atypical presentations
of pityriasis rosea: case presentations. J Eur Acad Dermatol Venereol.2005;
19: 120-126.
2. Braun-Falco O, Plewig G, Wolff HH, Burgdorf WHC. Dermatology:
Springer- Verlag,2000.pp584-5.
3. Balci DD, Hakverdi S. Vesicular pityriasis rosea: An
atypical presentation. Dermatol Online J 2008;14(3):6
4. Miranda SB, Lupi O, Lucas E. Vesicular pityriasis rosea:
response to erythromycin treatment. J Eur Acad Dermatol Venereol. 2004;18:622-5
5. Gonzalez LM, Allen R, janniger CK, Schwatz RA. Pityriasis
rosea: an important papulosqamous disorder. Int J Dermtol 2005;44:757-64
6. Parsons JM. Pityriasis rosea update. J Am Acad Dermatol
1986; 15: 159-167.
7. Fox C. Pityriasis rosea with vesiculation. Br J Dermatol
1906; 18: 281. Cross reference (cited by ref. 1)
8. Baker RJ, Johnson WC. Vesicular Pityriasis rosea. Cutis
1971;8:341-42. Cross reference (cited by ref. 4)
9. Anderson CR. Dapsone treatment in a case of vesicular
pityriasis rosea. Lancet 1971; 2: 493.
10. Chuang T, Perry HO, Ilstrup DM, Kurland LT. Recent
upper respiratory tract infection and pityriasis rosea: a case control study
of 249 matched pairs. Br J Dermatol 1983; 108: 587-591.
11. Labro MT. Anti-inflammatory activity of macrolides:
a new therapeutic potential? J Antimicrob Chemother 1998; 41 (Suppl B):
37-46info:pmid/6849825© 2011 Egyptian Dermatology Online Journal
|