|
|
Abstract
Pemphigoid gestationis is a rare autoimmune blistering disease
specific to pregnancy. It is characterized by pruritic, urticarial
plaques with development of tense vesicles and bullae within the
lesions. Recurrence with subsequent pregnancies are often more severe
and may be associated with miscarriages, prematurity, low birth weight
and rarely fetal death. We report this case of pemphigoid gestationis in
view of the importance of early diagnosis and treatment for prevention
of fetal risk.
Introduction
Pemphigoid gestationis (PG) is a rare autoimmune blistering disease
presenting almost exclusively during pregnancy [1],
though also associated with trophoblastic diseases [2].
It is a rare disease with an incidence of 1 in 50,000 pregnancies. PG
typically presents during the second or third trimester with recurrence
in subsequent pregnancies. It can be diagnosed by histopathology and
direct immunofluorescence which is confirmatory. Systemic steroids are
the mainstay of treatment.
Case report
A 25 year old normotensive, non-diabetic, euthyroid female, gravida
4, para 3, live children 2, with 24 weeks gestation presented with
severly pruritic eruption on limbs and trunk of 3 weeks duration. The
eruption started with severe pruritus over trunk and limbs followed two
days later by raised reddish lesions bilaterally on trunk and both upper
and lower limbs over a period of 2-3 days. Patient had similar but less
severe eruption in the last trimester of her third pregnancy, one year
back, and the baby died 3 days after a preterm vaginal delivery. The
patient had not taken any treatment that time except for some topical
preparations. She did not use oral contraceptives and did not report a
flare with her menses. There was no significant family or drug history.
Physical examination revealed bilaterally distributed erythematous
papules and plaques with a few target lesions and multiple tense bullae
and yellow crusted plaques on both forearms, diffuse vesicular plaques
over whole trunk including neck and multiple erythematous papules on the
thighs. Palms, soles and mucous membranes were not involved (Fig 1 &
2). Her haemogram, liver function tests, kidney function tests, TFT
and abdominal ultrasonography was normal. Tzank smear showed few
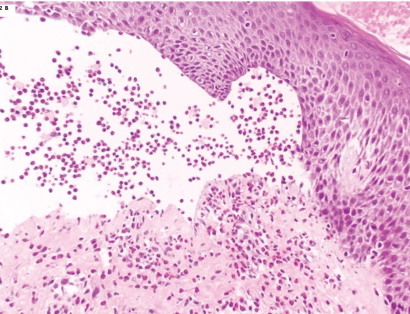
eosinophils. Skin biopsy results showed subepidermal vesicles and
papillary dermal edema. Scattered lymphocytes, histiocytes and
eosinophils were located in the dermis in a perivascular distribution
(Fig 3). DIF results showed fulorescence along dermo-epidermal
junction with anti C3.
 | Fig 1:
Papules and plaques with target lesions on abdomen. |
|
 | Fig
2: Tense bullae on forearm. |
|
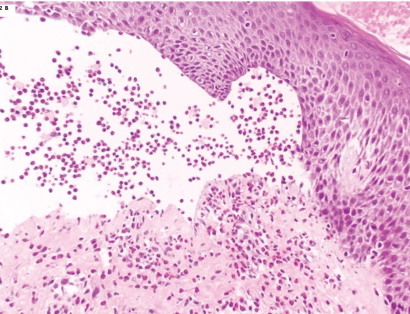 | Fig
3: H&E stain showing sub-epidermal vesicles containing
scattered lymphocytes, histiocytes and eosinophils. |
|
The patient was treated by oral prednisolone 40 mg daily for 1 week
and tapering 5mg every 5 days until a maintenance dosage of 20 mg daily
was achieved. The patient was also given chlorpheniramine 25 mg thrice
daily and topical mupirocin ointment for the crusted areas. The patient
was on regular follow up and maintenance dose of 20 mg daily till she
delivered and postpartum for 1 month. She delivered, vaginally at term,
a healthy baby.
Discussion
Pemphigoid gestationis is a rare dermatosis that almost exclusively
presents during pregnancy [1]. It has
also been associated with trophoblastic diseases such as hydatidiform
mole or choriocarcinoma [2]. The old
term herpes gestationis was coined in recognition of the herpetiform
lesions classically seen in PG [3] which
shares clinical, histological and immunological characteristics with
bullous pemphigoid [4]. PG is a rare
disease with an incidence of 1 in 50,000 to 60,000 pregnancies [5].
PG is an autoimmune blistering disease with autoantibodies of IgG1
and IgG4 subclass targeting BP 180 antigen and activate complement via
classical pathway [6]. The PG antigen is
located in the basement membrane of normal skin and in the basement
membrane zone of amniotic epithelium of both the placenta and umbilical
cord [7]. There appears to be a genetic
basis for the development of PG with HLA-DR3 and DR4. Recent
immuno-histochemical studies have identified a T-cell population with a
prevalent T helper (Th2) phenotype in the lesional skin of PG subjects,
which may be implicated in the recognition of self antigens and
production of pathogenic autoantibodies [8].
In PG, there is a sub-epidermal bulla with an overlying inflammatory
infiltrate consisting of histiocytes, lymphocytes and eosinophils in the
dermis. DIF shows deposition of C3 in a linear pattern along the
basement membrane and is considered pathognomic for diagnosis of PG [6].
In 25% to 30% of cases, IgG deposition also can be found along basement
membrane [9]. Powell et al [10]
demonstrated that a serological test measuring the major immunoreactive
portion of the NC 16A domain of BP 180 antigen can be used to verify the
diagnosis of PG and differentiate it from PUPPP.
Intense pruritus is the consistent hallmark of PG, while the clinical
course is variable. PG typically presents during the second or third
trimester with a mean onset of 21 weeks but may develop in the first
trimester, the time of delivery [6], the
first postpartum month [11], and with
the onset of menses or the use of oral contraceptives in the postpartum
period [12]. The clinical presentation
of PG is polymorphic with patients initially presenting with
erythematous papules, plaques or targetoid lesions followed by
appearance of small vesicles and bullae on normal skin or on top of
urticarial plaques. The PG lesions characteristically begin
peri-umbilically and then spread outward to include the buttocks, trunk
and extremities, sparing the mucous membranes, face, palms and soles [13].
Patients with PG should be identified as a high-risk pregnancy and be
followed accordingly. Fetal risks include miscarriages, prematurity, low
birth weight and rarely fetal death. Five to 10% of neonates have a
transient sub-epidermal blistering that resolves on its own with no
sequelae [14]. Systemic corticosteroids
remain the mainstay of treatment in the low dosage of 20- 60mg daily but
higher dosages up to 180 mg daily have been reported [11].
Maintenance therapy, generally at a lower dosage, may be required
throughout gestation and postpartum. Antipruritic drugs help to
alleviate pruritus. Dapsone, sulfapyridine, gold, cyclosporine,
methotrexate, cyclophosphamide, azathioprine, pyridoxine, IV
immunoglobulins and plasmapheresis have been tried with variable
results.
In conclusion, PG is an autoimmune disease occurring almost
exclusively during pregnancy. Its clinical course is variable but
eruptions typically respond to steroid therapy. It is important to
diagnose and treat PG early, not only to provide symptomatic relief to
patients but to avoid fetal risks.
References
1. Engineer L, Bhol K, Ahmad AR. Pemphigoid gestationis:
a review. AM J Obstet Gynecol 2000; 183: 483- 491.
2. Tillman WG. Herpes gestationis with hydatidiform mole
and chorion epithelioma. Br Med J 1950; 1: 1471.
3. Shornick JK. Herpes gestationis. J Am Acad Dermatol
1987; 17: 539-556.
4. Borradori L, saurat JH. Specific dermatoses of
pregnancy. Towards a comprehensive view. Arch Dermatol 1994; 130:
778-780.
5. Holmes RC, Black MM, Dann J, James DC, Bhogal B. A
comprehensive study of toxic erythema of pregnancy and herpes
gestationis. Br J Dermatol 1982; 106: 499-510.
6. Shornick JD. Dermatoses of pregnancy. Semin Cutan Med
Surg 1998; 17: 172-181.
7. Kelley SE, Bhogal BS, Wojnarowska F, Black MM.
Expression of a pemphigoid gestationis- related antigen by human
placenta. Br J Dermatol 1988; 118: 605-611
8. Fabbri P, Caproni M, Berti S, Bianchi B, Amato L, De
Pita O, et al. The role of T lymphocytes and cytokines in the
pathogenesis of pemphigoid gestationis. Br J Dermatol 2003; 148: 1141-8.
9. Kelley SE, Cerio R, Bhogal BS, Black MM. The
distribution of IgG subclass in pemphigoid gestationis: PG factor is an
IgG1 autoantibody. J Invest Dermatol 1989; 92: 695-698.
10. Powell AM, Sakuma-Oyama Y, Oyama N, Albert S,
Bhogal B, Kaneko F, et al. Usefulness of BP 180 NC16A enzyme -linked
immunosorbent assay in the serodiagnosis of pemphigoid gestationis (HG)
and differentiating between pemphigoid gestationis and pruritic
urticarial papules and plaques of pregnancy. Arch Dermatol 2005; 141:
705-710.
11. Jenkins RE, Hern S, Black MM. Clinical features and
management of 87 patients with pemphigoid gestationis. Clin Exp Dermatol
1999; 24: 255-259.
12. Holmes RC, Black MM, Jurecka W, Dann J, James DC,
Timulin D, et al. Clues to aetiology and pathogenesis of herpes
gestationis. Br J Dermatol 1983; 109: 131-139.
13. Shornick JK, Bangert JL, Freeman RG, Gilliam JN.
Herpes gestationis: clinical and histological features of 28 cases. J Am
Acad Dermatol 1983; 8: 214-224.
14. Shornick JK, Black MM. Fetal risks in Herpes
gestationis. J Am Acad Dermatol 1992; 26: 63-8.
© 2012 Egyptian Dermatology Online Journal
|