|
|
Abstract
Progressive symmetric erythrokeratoderma (PSEK) is a rare
genodermatosis with predominantly autosomal-dominant inheritance,
characterized by well demarcated, erythematous, hyperkeratotic plaques
that are symmetrically distributed over the extremities and buttocks,
and often the face. Like erythrokeratoderma variabilis, it doesn't have
seasonal variation. Here we are presenting a classical case of PSEK
having autosomal recessive inheritance with seasonal variation.
Introduction
Erythrokeratoderma (sometimes erythrokeratodermia) is the association
of localized hyperkeratotic plaques with overlapping or distinct areas
of circumscribed erythema. Many associations and possible syndromes are
reported. [1] Erythrokeratoderma has
both clinical and genetic heterogeneity. Currently, erythrokeratodermas
are divided into two major subtypes: EKV (erythrokeratoderma variabilis)
and PSEK (progressive symmetric erythrokeratoderma). [2]
Here we are presenting a classical case of progressive symmetric
erythrokeratoderma with seasonal variation.
Case history
A 22 year old male, product of second degree consanguineous marriage,
presented with palmo-plantar keratoderma and skin lesion. According to
his parents' statement the palmo-plantar keratoderma started at the age
of one year and noticed the skin lesions at the age of seven. It
initially started on the dorsa of hands and feet and spread over a
period of 2-3 months to involve the legs, knees and elbows and remained
static thereafter. The condition waxed and waned yearly without complete
resolution and became worse during winter season and nearly resolved by
summer leaving hyperpigmented lesions. There was no other triggering
factor involved and detailed history revealed no other affected members
of the family tree.
On examination multiple, well demarcated, bilaterally symmetrical
erythematous plaques with fine scaling of different geographical figures
were present over the dorsa of hands (fig 1), foot, legs (fig
2) and elbow region with palmo-plantar keratoderma (fig 3).
Abdomen, trunk, flexural areas and face were spared. The scalp, nail and
mucous membrane were normal.
 | Fig 1:
symmetric erythematous plaque on dorsum of hand. |
|
 | Fig
2: symmetric plaques on legs. |
|
 | Fig
3: plantar keratoderma. |
|
The general and systemic examinations of the patient were within
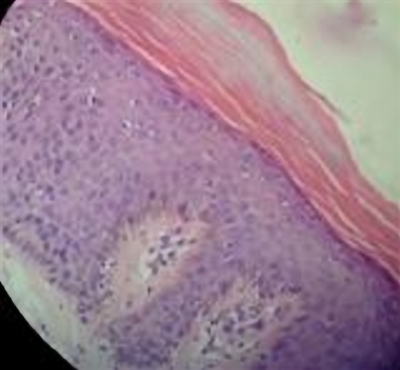
normal limits. Histopathology from the plaque over the knee region
revealed hyperkeratosis, normal granular layer and acanthosis with broad
rete ridges and in the dermis perivascular lymphocytic infilteration
(fig 4).
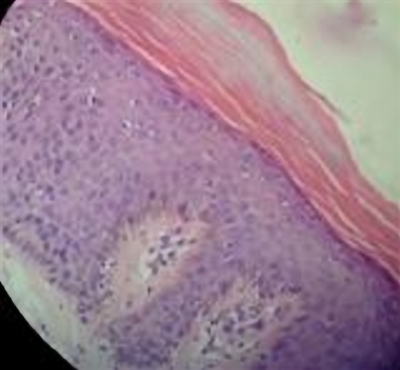 | Fig
4: Histopathological examination revealing hyperkeratosis,
normal granular layer and acanthosis with broad rete ridges and
in the dermis perivascular lymphocytic infiltration (H&E. 40x) |
|
A diagnosis of Progressive symmetric erythrokeratoderma was made
clinically and was consistent with the histopathological report.
Discussion
PSEK is a rare genodermatosis with predominantly autosomal-dominant
inheritance, although autosomal-recessive transmission has been also
observed.[3] Progressive symmetric
erythrokeratodermia was first described by Darier in 1911 and is
characterized by well demarcated, erythematous, hyperkeratotic plaques
that are symmetrically distributed over the extremities and buttocks,
and often the face. The trunk tends to be spared, but palms and soles
may be involved. [4] Onset usually
occurs during infancy with the development of slowly progressive non-
migratory erythematous plaques with scale. The plaques tend to progress
during childhood, with lesions stabilizing thereafter. [2]
Genetic analyses of large affected families, in conjunction with
studies in transgenic mice, have suggested the loricrin gene is
associated with the features of this disease. Loricrin is the major
structural component of the cornified cell envelope that is formed
beneath the plasma membrane of stratified squamous epithelial cells
during terminal differentiation. [5]
The diagnosis is invariably clinical, as loricrin gene analysis is
difficult in hospital settings. [4]
Erythrokeratoderma variabilis (EKV) which may resemble PSEK differs
from the latter, as the lesions of EKV continuously changes and may be
induced by external mechanical pressure and temperature changes. [6]
Progressive symmetrical erythrokeratoderma (PSEK), resemble those of
EKV, but migratory erythema is not seen. Facial involvement and
palmoplantar keratoderma are more characteristic of PSEK. [2]
In our case there was an autosomal recessive pattern of inheritance,
with palmoplantar keratoderma since infancy and symmetric lesions over
skin with waxing and waning without complete resolution.
In conclusion, we hereby present a rare and a classical case of
progressive symmetric erythrokeratoderma with seasonal variation.
References
1. Judge MR, McLean WHI, Munro CS. Disorders of
keratinisation. In: Burns T, Breathnach S, Cox N, Griffiths C, editors.
Rook's textbook of Dermatology. 8th ed.Wiley Blackwell; 2010. p19.69.
2. Hirano SA, Harvey VM. From progressive symmetric
erythrokeratoderma to erythrokeratoderma variabilis progressive. J Am
Acad Dermatol 2010; 64(5): e81-e82.
3. Yan H, Zhang J, Liang W, Zhang H, Liu J. Progressive
symmetric erythrokeratoderma: Report of a Chinese family. Indian J
Dermatol Venereol Leprol 2011; 77: 597- 600.
4. Fleckman P, DiGiovanna JJ. The Icthyosis. In: Wolff
K, Goldsmith LA, Katz SI, Gilchrist BA, Paller AS, Leffell DJ, editors.
Fitzpatrick s Dermatology in General Medicine.7th ed. New York: McGraw
Hill; 2008. p.418.
5. Chu DH, Arroyo MP. Progressive and symmetric
erythrokeratoderma Dermatology Online Journal 2003;9(4): 21
6. Beare JM, Nevin NC, Frogatt P, Kernohan DC, Allen IV.
Atypical erythrokeratodermia with deafness, physical retardation and
peripheral neuropathy. Br J Dermatol 1972; 87: 308- 14.
© 2012 Egyptian Dermatology Online Journal
|