Abstract
Background Human immuno-deficiency virus (HIV) affects every strata of society but the illiterate and economically backward people are the most affected. When children with HIV develop clinical manifestations and need treatment, they have to travel from faraway places to access care and management at tertiary institutions. This leads to either non-compliance with treatment or wastage of meagre resources of the patient.
Methods Four hundred children diagnosed with HIV/AIDS coming to the Department of Dermatology in a hospital in North India for diagnosis and treatment of various skin disorders were questioned with respect to their family's social, economic and educational background. Demographic variables such as age, sex, education, occupation and data on clinical manifestations were reviewed.
Results Out of the 400 children, males outnumbered females in the ratio of 1.96:1. Most of the children were in the age group of 10-15 years (55.75%) and the majority belonged to rural areas (88.25 %). Most of the children were going to school in the standards appropriate for their age. The most common mucocutaneous manifestations in these children were oral candidiasis (10%), staphylococcal skin infections (12.5%) and pruritic papular eruptions (12.5%).
Conclusion The common mucocutaneous manifestations must be considered as markers of HIV and should prompt the clinician to get HIV status tested. The primary and secondary health care centres should have trained personnel to diagnose and treat HIV disease and opportunistic infections so as the children to have much needed care and support nearer to home.
Introduction
With the availability of antiretroviral therapy (ART), human immunodeficiency virus (HIV) infection, which was once considered a progressively fatal illness, has now become a chronic treatable condition in children, as in adults. However, as children have their whole life ahead of them, they face far more overwhelming challenges. The most significant inadequacy in the response to paediatric HIV remains the insufficient prevention of mother-to-child transmission (PMTCT), allowing a large number of children to be born with HIV in the first place, in spite of it being largely preventable.[1] HIV infection poses tremendous challenges to health globally. According to the latest estimates from UNAIDS, in 2011, there were 34.2 million people living with HIV throughout the world. Out of these, 3.4 million were children.[2] In India, the number of people affected by HIV/AIDS were 23,95,442 out of which 1,04,450 were children.[3] The universal access to comprehensive health services is focused to address six needs: voluntary counselling and testing, prevention of HIV transmission, prophylaxis against opportunistic infections (OI), diagnosis and treatment for OIs and neoplasms, anti retroviral therapy (ART), palliative care and health care infrastructure and capacity to provide quality care.[4] These services have however, not taken into account, the pattern of socio-demographical factors which have a significant impact on patient's compliance and behaviour. The HIV infected people need to travel long distances to access care in tertiary level hospitals. This is especially troublesome for the children living with HIV/AIDS, who are entirely dependent on surviving parents, grandparents or guardians for care and treatment. The clinical presentation of HIV infection in children has been reported in various studies. However, large and reliable data on socio-demographic parameters are still inadequate.
Materials and Methods
For the present study, 400 children previously diagnosed with HIV/AIDS reporting to the Department of Dermatology of a North Indian Hospital for the diagnosis and treatment of skin diseases were studied. Appropriate clearance was obtained from the ethical committee of the college before initiation of the study. After taking an informed consent, complete history of the patient was taken with due regard to demographic and social parameters. This was followed by general physical examination, systemic examination and mucocutaneous examination. The relevant investigations, depending on the disease and the presentation, were carried out. The CD4 count, measured by flow cytometry, was done. All the details were recorded on a prescribed proforma and data obtained were compiled and analysed.
Results
In this study conducted over a period of 2 years, 400 children were enrolled and examined. Out of these, male cases outnumbered female cases i.e. 265 male cases (66.25%) as compared to 135 female cases (33.75 %). Male to female ratio was 1.96:1
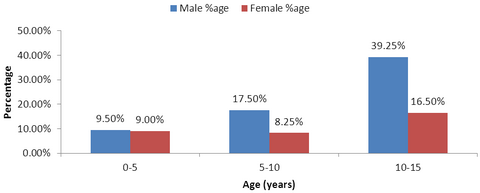
(Table 1). The maximum number of cases were in the age group of 10-15 years i.e. 223 (55.75%) cases, the range being 18 months to 15 years
(Fig 1 and Table 2) Also, when the age and sex distribution were analysed simultaneously, it was seen that the ratio of male and female children were almost the same in the age group of 0-5 years. With increasing age, the disparity between the two sexes increased, and in the age group of 5-10 years, males were almost double that of females (17.50% males, 8.25% females).Between 10-15 years, males outnumbered females even more (39.25% males vs 16.5% females)
(Fig 1). There was preponderance of rural cases i.e. 353 (88.25 %) cases as compared to 47 (11.75%) urban cases which was expected in an agricultural state like Punjab
(Table 3). Also, the maximum number of children belonged to Punjab i.e. 386 (96.5%) cases and only 14 (3.5%) cases were from families of migrants (Non-Punjabi) who came from other parts of India in search of livelihood
(Table 4). Most of the children included in this study were going to primary school i.e. 178 (44.5%) cases followed by secondary school i.e. 127 (31.75%) cases. Some children had dropped out of school i.e. 19 (4.75%) due to various reasons and some younger children i.e. 76 (19%) had not started going to school yet
(Table 5). Mother to child transmission (MTCT) was the predominant mode of transmission in 393 (98.25%) patients in the present study followed by parenteral route in 7 cases (1.75%) which included transmission through contaminated needles and blood transfusion. No case of transmission of HIV through sexual contact or due to injection drug abuse was seen in this study. Also there were no cases where the source of infection to the child was unidentified.
(Table 6)
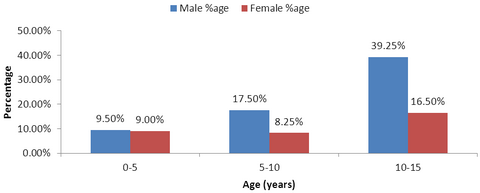 | Fig 1:
Age And Sex Wise Distribution |
|
The most common clinical manifestations among infections was oral candidiasis i.e. 40 cases (10%) followed by furunculosis in 26 cases (6.5 %), impetigo in 24 (6%) cases, molluscum contagiosum and pediculosis capitis in 18 cases each (4.5%), verruca vulgaris in 15 cases (3.75%), dermatophyte infection in 20 cases (5.00%). Other common manifestations seen were scabies, herpes simplex virus infections and cutaneous candidiasis
in 9 cases each (2.25%). (Table 7) The most common clinical manifestations among non infectious dermatoses was pruritic papular eruptions (12.5%) followed by seborrheic eczema in 6.5%,other eczemas in 4.75%, generalized itching with xerosis (3.25%) and cutaneous drug eruptions (3.5%). Recurrent aphthous stomatitis was seen in 1.25% and angular cheilitis
in 1.5% of the total patients. Pigmentation of nails was observed in 2.25%
and diffuse alopecia was seen in 1.25 % of the patients. (Table 8)
|
Sex |
No. of cases |
Percentage |
|
Male |
265 |
66.25% |
|
Female |
135 |
33.75% |
|
Total |
400 |
100 |
Table 1: Sex Wise Distribution
|
Age (years) |
No. of cases |
Percentage |
|
0-5 |
74 |
18.50% |
|
5-10 |
103 |
25.75% |
|
10-15 |
223 |
55.75% |
|
Total |
400 |
100.00% |
Table 2: Age Wise Distribution
|
Rural/ Urban |
No. of cases |
Percentage |
|
Rural |
353 |
88.25% |
|
Urban |
47 |
11.75% |
|
Total |
400 |
100.00% |
Table 3:
Rural & Urban Distribution
|
Punjabi/Non-punjabi |
No. of cases |
Percentage |
|
Punjabi |
386 |
96.50% |
|
Non-Punjabi(Migrant) |
14 |
3.50% |
|
Total |
400 |
100.0 |
Table 4:
Punjabi & Non-punjabi Status
|
Level of education |
No. of cases |
Percentage |
|
Preschool |
76 |
19.00% |
|
Primary |
178 |
44.50% |
|
Secondary |
127 |
31.75% |
|
School dropouts |
19 |
4.75% |
|
Total |
400 |
100.0 |
Table 5:
Educational Status
|
|
No. of cases |
Percentage |
|
Mother to child(Vertical) |
393 |
98.25% |
|
Parenteral (blood transfusion & infected needles) |
7 |
1.75% |
|
Sexual contact/abuse |
0 |
0 |
|
Unknown |
0 |
0 |
|
Total |
400 |
100.0 |
Table 6:
Route of Transmission
|
Infectious dermatoses |
Male |
Female |
Total |
|
No. of cases |
%age |
No. of cases |
%age |
No. of cases |
%age |
|
BACTERIAL INFECTIONS |
|
Impetigo |
13 |
3.25% |
11 |
2.75% |
24 |
6.00% |
|
Furunculosis |
20 |
5.00% |
6 |
1.50% |
26 |
6.50% |
|
Other pyodermas |
4 |
1.00% |
2 |
0.50% |
6 |
1.50% |
|
Cutaneous TB |
0 |
0 |
1 |
0.25% |
1 |
0.25% |
|
VIRAL INFECTIONS |
|
Molluscum contagiosum |
12 |
3.00% |
6 |
1.50% |
18 |
4.50% |
|
Herpes simplex infections |
5 |
1.25% |
4 |
1.00% |
9 |
2.25% |
|
Herpes zoster |
5 |
1.25% |
|
0.00% |
5 |
1.25% |
|
Verruca vulgaris |
12 |
3.00% |
3 |
0.75% |
15 |
3.75% |
|
Epidermodysplasia verruciformis |
1 |
0.25% |
|
0.00% |
1 |
0.25% |
|
Genital/ Perianal warts |
2 |
0.50% |
|
0.00% |
2 |
0.50% |
|
FUNGAL INFECTIONS |
|
Oral candidiasis |
24 |
6.00% |
16 |
4.00% |
40 |
10.00% |
|
Dermatophytosis |
13 |
3.25% |
7 |
1.75% |
20 |
5.00% |
|
Pityriasis versicolor |
4 |
1.00% |
0 |
0.00% |
4 |
1.00% |
|
Candidiasis |
6 |
1.50% |
3 |
0.75% |
9 |
2.25% |
|
PARASITIC INFECTIONS |
|
Scabies |
8 |
2.00% |
1 |
0.25% |
9 |
2.25% |
|
Pediculosis |
6 |
1.50% |
12 |
3.00% |
18 |
4.50% |
Table 7: Infectious Mucocutaneous Manifestations
|
Non Infectious dermatoses |
Male |
Female |
Total |
|
No. of cases |
%age |
No. of cases |
%age |
No. of cases |
%age |
|
Pruritic papular eruptions |
33 |
8.25% |
17 |
4.25% |
50 |
12.50% |
|
Seborrheic eczema |
21 |
5.25% |
5 |
1.25% |
26 |
6.50% |
|
Cutaneous drug reactions |
6 |
1.50% |
8 |
1.75% |
14 |
3.50% |
|
Xerosis |
9 |
2.25% |
4 |
1.00% |
13 |
3.25% |
|
Aphthous stomatitis |
4 |
1.00% |
1 |
0.25% |
5 |
1.25% |
|
Angular cheilitis |
5 |
1.25% |
1 |
0.25% |
6 |
1.50% |
|
NAIL CHANGES |
|
|
|
|
|
|
|
Leukonychia |
9 |
2.25% |
4 |
1.00% |
13 |
3.25% |
|
Melanonychia |
8 |
2.00% |
1 |
0.25% |
9 |
2.25% |
|
HAIR CHANGES |
|
|
|
|
|
|
|
Diffuse alopecia |
4 |
1.00% |
1 |
0.25% |
5 |
1.25% |
|
Alopecia areata |
3 |
0.75% |
1 |
0.25% |
4 |
1.00% |
|
Telogen effluvium |
0 |
0.00% |
3 |
0.75% |
3 |
0.75% |
|
Hypopigmented brittle hair |
3 |
0.75% |
4 |
1.00% |
7 |
1.75% |
|
Trichomegaly |
0 |
0 |
2 |
0.50% |
2 |
0.50% |
|
Other Eczemas |
14 |
3.50% |
5 |
1.00% |
19 |
4.75% |
|
Acne vulgaris |
2 |
0.50% |
|
0.00% |
2 |
0.50% |
|
Generalised hyperpigmentation |
6 |
1.50% |
4 |
1.00% |
10 |
2.50% |
|
Lichen planus |
1 |
0.25% |
0 |
0 |
1 |
0.25% |
|
Urticaria |
2 |
0.50% |
2 |
0.50% |
4 |
1.00% |
Table 8: Non Infectious Mucocutaneous Manifestations
Discussion
Children affected by HIV/AIDS have to face many problems at their tender age. HIV/AIDS predisposes them to opportunistic infections leading to significant morbidity and mortality. In addition, the parents of the child, themselves suffering from HIV/AIDS, may not be able to provide proper nutrition and treatment for the child. In case the parents of the child die due to AIDS or other illness, the child becomes orphan and is left to fend for himself. These children are forced to live a life of poverty and may thus fall prey to antisocial elements of the society. According to WHO, at the end of 2010, there were 3.4 million children living with HIV around the world. An estimated 390,000 children became newly infected with HIV in 2010. In 2011, 330,000 new infections occurred among children, which was a decrease of 24% than 2009 but still, HIV was responsible for 230,000 deaths among children. [2] In the absence of prophylactic antiretroviral therapy to the mother during pregnancy, labour and delivery and to the fetus following birth, the probability of transmission of HIV from mother to fetus ranges from 15-25% in industrialized countries and from 25-35% in developing countries.[5] In India, the estimated vertical transmission would be at the rate of 30 per cent and would expect to have 75000 infected neonates born every year.[6] Education and the socio-economic status are major components of health seeking behaviour. While clinical presentations and treatment modalities of AIDS are widely discussed, the focus has hardly ever been on the needs of the patient. A child living alone or with diseased guardians can hardly ever cover large distances solely for treatment purposes. The European Collaborative Study reported that more than 15 per cent of infected children will have progressed to category C or death by the age of 1 year and nearly 50 per cent by 10 years. Just fewer than 20 per cent of children will have evidence of severe immunodeficiency by the age 1 and 75 per cent by 10 years of age.[7] Skin is one of the most frequently involved organs in HIV infection and it is involved early in the course of the disease. Hence, mucocutaneous manifestations may be one of the earliest markers of HIV/AIDS.[8] As skin has the particular advantage of presenting with clearly visible and easily accessible disorders, their diagnosis and accurate suspicion of HIV can go a long way in early detection of AIDS. In the present study, the most common infectious dermatosis was oral candidiasis which was seen in 10% patients. In other similar studies, the incidence was found to be 25.6% and 33%.[9,10] The most common non infectious dermatosis was pruritic papular eruption which was seen in 12.5% patients. This observation is in agreement with the outcome of the works of Lim et al [11] and Wananakul and Thisyakorrn.[12] A similar study on the socio- demographic factors was done in Chennai, India, and their socio-demographic profile was comparable to our results.[13] This emphasises the uniformity in the pattern of HIV afflicted children throughout the country and rather the world. Also, it reiterates the need for further studies on the subject so that policy framework may be designed in accordance to the patient needs.
Conclusion
The menace of HIV is more profound in children due to its effect on social standing and upbringing of the child. With clear knowledge of the socio-demographic factors affecting HIV positive children along with the added knowledge of significant mucocutaneous manifestations, it may become possible to provide early, adequate and holistic treatment to these children at a centre in close proximity to their native place. References
1. Mothi SN, Karpagam S, Swamy VHT, Mamatha ML, Sarvode SM. Paediatric HIV - trends & challenges. Indian J Med Res 2011;134(6): 912-19.
2.
UNAIDS fact sheet. [Online] 2012 Jul. [cited 2012 Oct 23] Available from:
URL: http://www.unaids.org/en/media/unaids/contentassets/
documents/epidemiology/2012/201207_FactSheet_Global_en.pdf.
3. NACO
fact sheet. [Online] 2012 Mar [cited 2012 Oct 23] Available from: URL:
http://www.nacoonline.org/Quick_Links/Publication/State_Fact_Sheets
/Fact_Sheets/State_Fact_Sheet_-_March_2012/ .
4. Kitahata MM, Tegger MK, Wagner EH, Holmes KK.Comprehensive health care for people infected with HIV in developing countries. BMJ 2002;325 : 954-7.
5. Douglas GC, King BF. Maternal fetal transmission of human immunodeficiency virus: a review of possible routes and cellular mechanisms of infection. Clin Infect Dis 1992;15(4):678-91.
6. Kapoor A, Kapoor A, Vani SN. Prevention of mother-to-child transmission of HIV. Indian J Pediatr 2004;71 : 247-51.
7. European Collaborative Study. Fluctuations in symptoms in human immunodeficiency virus-infected children: The first 10 years of life. Pediatrics 2001;108 :116-22.,.
8. Mendiratta V, Mittal S, Jain A, Chander R. Mucocutaneous manifestations in children with human immunodeficiency virus infection. Indian J Dermatol Venereol Leprol 2010;76:458-66.
9. Umoru Dominic et al. Mucocutaneous manifestation of pediatric human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) in relation to degree of immunosuppression: a study of a West African population. International Journal of Dermatology 2012; 51(3):305-12.
10. Wananukul Siriwan et al.Mucocutaneous Findings in Pediatric AIDS Related to Degree of Immunosuppression. J Pediatric Dermatology 2003;20(4): 289-94.
11. Lim W, Sadick N, Gupta A, et al. Skin diseases in children with HIV infection and their association with degree of immunosuppression. Int J Dermatol 1990;29: 24-29.
12. Wananukul C, Thisyakorrn U. Mucocutaneous manifestations of HIV infection in 91 children born to HIV-seropositive women.Pediatr Dermatol 1999;16: 359-63.
13. Rajasekaran S, Jeyaseelan L, Raja K, Ravichandran N. Human immunodeficiency virus (HIV) infection poses tremendous challenges to health globally. Demographic & clinical profile of HIV infected children accessing care at Tambaram, Chennai, India. Indian J Med Res Jan 2009;129:42-9.© 2013 Egyptian Dermatology Online Journal |