|
|
Introduction
Gorlin syndrome or nevoid basal cell carcinoma syndrome (NBCCS) is a
rare autosomal dominant disorder with complete penetrance but variable expressivity.
It affects nervous system, eyes, endocrine system and bones and characterized
by multiple basal cell carcinomas (BCC), odontogenic keratocyst, characteristic
facial appearance, skeletal abnormalities and malignancies of various organs.
The prevalence is reported to be 1 case per 56,000-164,000 population [1,2].
Recent work has shown NBCCS to be caused by mutations in the tumor suppressor
gene, PTCH1 (patched) gene found on chromosome 9q22.3. Approximately 60
percent of patients with a diagnosis of Gorlin syndrome are expected to
have a mutation in the PTCH gene identifiable by sequencing [3].
Herein, we report a case of 40 year female with many important clinical
findings of nevoid basal cell carcinoma syndrome.
Case Report
A 40 year female presented with 12 years history of multiple pigmented
lesions on the upper limbs, lower limbs and face. These lesions were initially
small in size and suddenly increased in size since 6 months. On examination
these were multiple darkly pigmented lesions of variable sizes ranging from
0.5cm to 2.5cm (Fig 1a). Few of these were ulcerated and crusted
(Fig 1b).
There is no evidence of local bone involvement or distant metastasis. The
patient had hypertelorism and macrocephaly. Numerous tiny pits were observed
on palms and soles. She had a past history of operation for ovarian tumor
10 years back. The histopathology of the ovarian mass revealed fibroma.
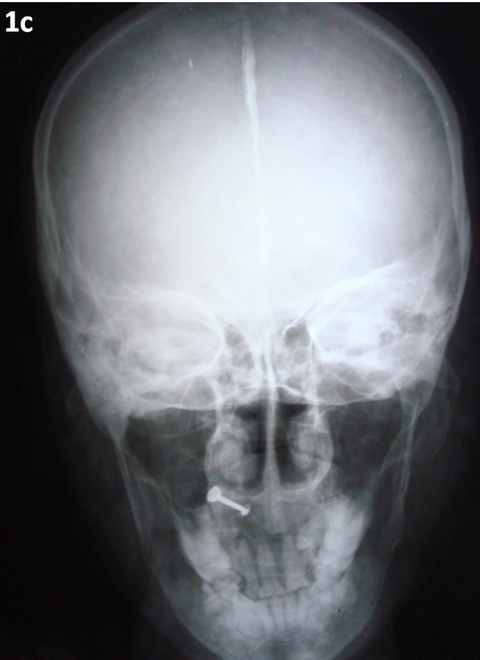
Radiograph of skull and vertebrae showed calcification of falx cerebri
(Fig 1c)
and mild scoliosis. CT scan of the brain and ultrasound scan of the abdomen
did not reveal any abnormality. Her mother and grand mother also had similar
pigmented skin lesions. With these features the clinical diagnosis was made
to be nevoid basal cell carcinoma syndrome.
 | Fig 1a:
Multiple darkely pigmented lesions on face |
|
 | Fig 1b:
An ulcerated lesion on thigh |
|
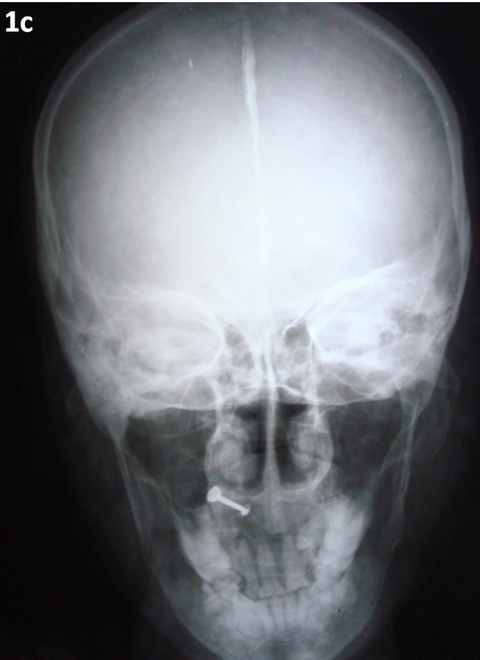 | Fig 1c:
x-Ray showing calcification of falx cerebrie |
|
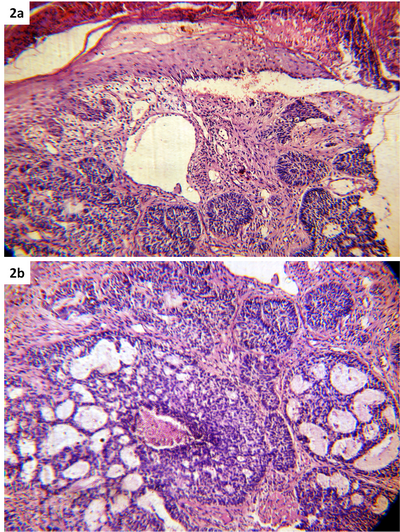
Histopathological examination of a representative specimen from one of
the pigmented lesion showed tumor nests consisting of basaloid cells having
mild cellular and nuclear atypia and arranged in a palisading fashion, dispersed
throughout the dermis (Fig 2a). Few areas showed cribiform pattern
(Fig 2b).
These histological findings were consistent with basal cell carcinoma. These
histological findings were consistent with our clinical diagnosis of nevoid
basal cell carcinoma syndrome.
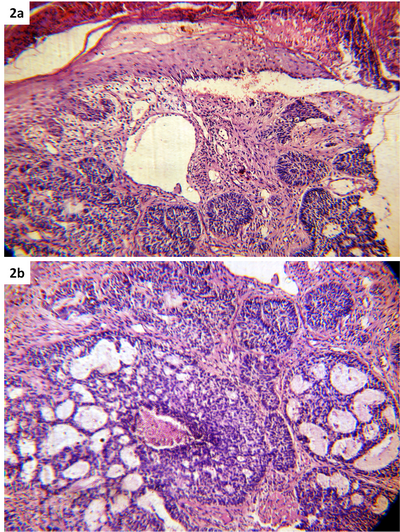 | Fig
2: Biopsy showing basaloid cell nest in dermis (a)
and cribiform pattern (b) (H&E X 200) |
|
Gorlin syndrome should be differentiated from other conditions with multiple
basal cell carcinomas. These include Bazex syndrome and Rombo syndrome.
Hair shaft abnormalities along with atrophoderma are common in Bazex syndrome
and trichoepethelioma in Rombo syndrome, which are not seen in Gorlin syndrome
[1].
Gorlin syndrome was first described by Gorlin and Goltz in 1960 [4].
Kimonis et al. have proposed the criteria for the diagnosis of Gorlin syndrome
[5]. The characteristic findings in this
condition are multiple BCCs, palmar and plantar pits, jaw cysts, bony abnormalities,
and medulloblastoma. Multiple jaw keratocysts are frequently begun in the
second decade of life with the mandible more commonly involved than the
maxilla. Usually these cysts are asymptomatic; however, they may cause dental
pain and swelling when they erode the bone. Histologically these cysts are
odontogenic keratocysts . Basal cell carcinomas also appear early in life,
usually in the third decade onwards and are numerous. However, the appearance
of numerous BCCs at an early age and over sites not exposed to sunlight
differentiates it from others. Palmar and plantar pits represent an aborted
or immature attempt to form BCC. They are more visible on hands and feet
after immersion in warm water for a few minutes. Other skin manifestations
include facial milia, which can be numerous, and meibomian cysts in the
eyelids. Sebaceous cysts and dermoid cysts are also common. Skin tags (especially
around the neck) often have the histological appearance of BCCs but do not
act aggressively. Approximately 60% of individuals have a recognizable appearance
with macrocephaly, bossing of the forehead, coarse facial features. Most
individuals have skeletal anomalies (e.g., bifid ribs, wedge-shaped vertebrae).
Ectopic calcification, particularly in the falx, is present in more than
90% of affected individuals by age 20 years. Cardiac and ovarian fibromas
occur in approximately 2% and 20% of individuals respectively. Cardiac fibromas
are usually present at birth or soon after. They are mostly asymptomatic,
but can cause arrhythmia or obstruction of cardiac flow, may cause torsion
of the ovary but are not thought to affect fertility. Malignant transformation
in ovarian fibroma is uncommon. Rhabdomyomas may occur at other sites as
well as in the heart. Approximately 5% of children with NBCCS develop medulloblastoma
(primitive neuroectodermal tumor [PNET]), generally the desmoplastic subtype.
Peak incidence is at age two years [6].
Life expectancy in NBCCS is not significantly different from average. The
major problem is with the cosmetic effect of the treatment of multiple BCCs
and to a lesser extent with dental cysts.
In conclusion, Gorlin syndrome is often not diagnosed in childhood as
many of the characteristic features develop later in life. Couples with
a family history of this syndrome might consider genetic counseling before
becoming pregnant. Frequent follow-up with doctors of various specialties
is vital to achieve a good outcome.
References
1. Oro AE. Basal cell Nevus syndrome In: Fitzpatrick's Dermatology
in General Medicine Wolff K, Goldamith LA, Katz SI et al edrs, 7th edn,
McGraw-Hill, NewYork 2008:1042-48.
2. Totten JR. The multiple naevoid basal cell carcinoma
syndrome. Cancer 1980; 46:1456-62.
3. K N Shivaswamy, T K Sumathy, A L Shyamprasad, C Ranganathan:
Gorlin syndrome or basal cell nevus syndrome (BCNS): A case report. Dermatology
Online Journal September 2010;16 (9): 6.
4. Gorlin RJ, Goltz RW. Multiple nevoid basal cell epithelioma,
jaw cysts and bifid rib. A syndrome. N Engl J Med 1960; 262:908-912.
5. Kimonis VE, Goldstein AM, Pastakia B, Yang ML, Kase R,
DiGiovanna JJ, et al. Clinical manifestations in 105 persons with nevoid
basal cell carcinoma syndrome. Am J Med Genet.1997;69(3):299-308.
6. K Patil, VG Mahima, B Gupta. Gorlin syndrome: A case
report. J of Ind society of pedodontics and preventive dentistry 2005; 23
(4): 198-203.© 2013 Egyptian Dermatology Online Journal
|