|
|
Abstract
Sexually transmitted infections (STIs) are a known risk factor for
Human Immunodeficiency Virus (HIV) transmission, with reference to both
susceptibility to infection and infectivity. Both ulcerative and
non-ulcerative inflammatory STIs are associated with an increased risk
of HIV transmission.
Out of all the patients reporting to STI/ RTI (Reproductive Tract
Infection) clinic, 1000 patients with symptoms and clinical features of
STI/RTI were examined. The data were collected on a prescribed proforma
and were analyzed statistically. In our study, the highest number of
female patients had bacterial vaginosis i.e. 244 patients (38.2%),
followed by 205 females (32.1%) having candidial vulvovaginitis.
Forty-seven females (7.4%) had cervicitis, 29 (4.5%) had herpes
genitalis, 26 (4.1%) had ano-genital warts, 21 (3.3%) had molluscum
contagiosum while 12 females (1.9%) were diagnosed to have pelvic
inflammatory disease.
Among the male patients, balanoposthitis was the most common STI,
seen in 136 patients (37.6%), followed by herpes genitalis in 91 (25.1%)
patients, anogenital warts in 47 males (13.0%), and molluscum
contagiosum in 28 (7.7%) patients. To conclude, infective bacterial and
fungal STIs constitute the major burden at the STI/RTI clinics.
Syndromic management i.e. treatment based on easily identifiable
symptoms and signs (syndrome) is useful for tackling the increasing
burden of STIs. It is a comprehensive approach. The basis of this
approach is the fact that many sexually transmitted pathogens are known
to produce similar clinical features. [1]
Introduction
Sexually transmitted diseases are the most formidable enemy of human
race; enemies entrenched behind the strongest human passion and deepest
social tragedies. The population explosion, migration of rural
population to urban centers and increasing promiscuity have all led to
enormous spread of sexually transmitted diseases in the community. [1]
Methods
The present study comprised of 1000 patients with STI/RTIs attending
the department of Dermatology, Venereology and Leprosy and the
department of Obstetrics and Gynaecology of Guru Nanak Dev Hospital
attached to Government Medical College, Amritsar.
A detailed history was taken which included any history of premarital
/ extramarital sexual contact, blood transfusion, intra-venous drug use
and was recorded on a proforma. It was followed by general physical
examination and mucocutaneous examination. The data collected were
analyzed statistically to know the clinico-epidemiological profile of
the 1000 cases.
Results
Table 1 shows the demographic profile of the study patients.
Among the 1000 studied cases, the majority were females i.e. 638 (63.8%)
while males were 362 (36.2%) in number. The majority of cases were in
the 16-30 years age group i.e. 464 (46.4%) cases, followed by 31-45
years age group i.e. 426 cases (42.6%).
|
Demographic Features |
No. of patients |
% |
|
Gender |
|
Male |
362 |
36.2 |
|
Female |
638 |
63.8 |
|
Rural/Urban Distribution |
|
Rural |
390 |
39 |
|
Urban |
610 |
61 |
|
Age (in years) |
|
<15 |
0 |
0 |
|
16-30 |
464 |
46.4 |
|
31-45 |
426 |
42.6 |
|
45-60 |
108 |
10.8 |
|
>60 |
2 |
0.2 |
|
0ccupational Status |
|
House wife |
498 |
49.8 |
|
Farmer |
81 |
8.1 |
|
Govt. employee |
73 |
7.3 |
|
Unskilled worker |
84 |
8.4 |
|
Skilled worker |
154 |
15.4 |
|
Driver |
26 |
2.6 |
|
Student |
39 |
3.9 |
|
Others |
45 |
4.5 |
|
History of pre/extra- marital sexual contact |
|
Present |
263 |
26.3 |
|
Absent |
737 |
73.7 |
|
Marital status |
|
Married |
904 |
90.4 |
|
Unmarried |
67 |
6.7 |
|
Widow |
24 |
2.4 |
|
Divorcee |
5 |
0.5 |
Table 1: Showing demographic profile Of 1000 study cases
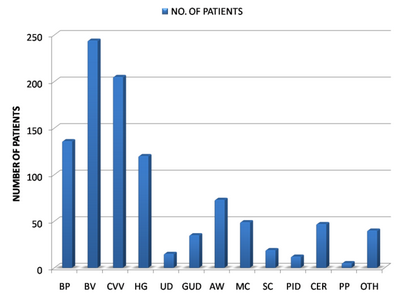
In our study, the highest number of female patients had bacterial
vaginosis i.e. 244 patients (38.2%), followed by 205 females (32.1%)
having candidial vulvovaginitis. Forty-seven females (7.4%) had
cervicitis, 29 (4.5%) had herpes genitalis, 26 (4.1%) had ano-genital
warts, 21 (3.3%) had molluscum contagiosum while 12 females (1.9%) were
diagnosed to have pelvic inflammatory disease {Table 2 and Fig 1}.
Among the male patients, balanoposthitis was thevmost common seen in
136 patients (37.6%), followed by herpes genitalis in 91 (25.1%)
patients, anogenital warts in 47 males (13.0%), and molluscum
contagiosum in 28 (7.7%) patients {Table 2 and Fig 1}.
|
Clinical Diagnoses |
Male |
Female |
Total |
|
No. of cases |
%age |
No. of cases |
%age |
No. of cases |
%age |
|
Balanoposthitis (BP) |
136 |
37.6 |
0 |
0 |
136 |
13.6 |
|
Bacterial vaginosis (BV) |
0 |
0 |
244 |
38.2 |
244 |
24.4 |
|
Candidial Vulvovaginitis (CVV) |
0 |
0 |
205 |
32.1 |
205 |
20.5 |
|
Herpes genitalis (HG) |
91 |
25.1 |
29 |
4.5 |
120 |
12 |
|
Urethral discharge (UD) |
13 |
3.6 |
2 |
0.3 |
15 |
1.5 |
|
Genital ulcer disease (GUD) |
23 |
6.4 |
12 |
1.9 |
35 |
3.5 |
|
Anogenital warts (CA) |
47 |
13 |
26 |
4.1 |
73 |
7.3 |
|
Molluscum contagiosum (MC) |
28 |
7.7 |
21 |
3.3 |
49 |
4.9 |
|
Scabies (SC) |
19 |
5.2 |
0 |
0 |
19 |
1.9 |
|
Pelvic inflammatory disease (PID) |
0 |
0 |
12 |
1.9 |
12 |
1.2 |
|
Cervical erosion (CER) |
0 |
0 |
47 |
7.4 |
47 |
4.7 |
|
Pediculosis pubis (PP) |
5 |
1.4 |
0 |
0 |
5 |
0.5 |
|
Non- specific discharge (NS) |
0 |
0 |
40 |
6.3 |
40 |
4 |
|
Total |
362 |
100 |
638 |
100 |
1000 |
100 |
Table 2: showing the clinical diagnosis in 1000 study cases
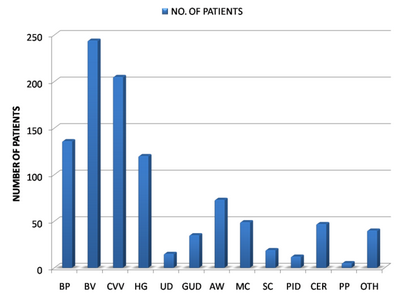 | Fig 1:
Graph showing diagnosis in the 1000 study cases.
[Balanoposthitis (BP), Bacterial vaginosis (BV), Candidial
Vulvovaginitis (CVV), Herpes genitalis (HG), Urethral discharge
(UD), Genital ulcer disease (GUD), Anogenital warts (CA),
Molluscum contagiosum (MC), Scabies (SC), Pelvic inflammatory
disease (PID), Cervical erosion (CER), Pediculosis pubis (PP),
Non- specific discharge (NS)]. |
|
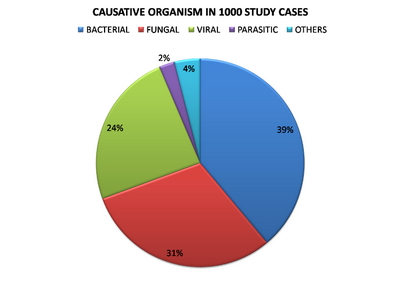
Figure 2 shows the type of organism responsible for the
STI/RTI in studied cases.
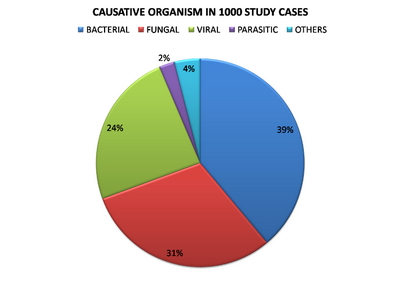 | Fig
2: Showing the type of causative organisms responsible for
STI/RTI among the study cases. |
|
In our study, 124 patients (12.4%) were found to be positive for
HIV-1 antibodies while no patient was found to be positive for HIV-2
antibodies.
Discussion
India has a population of more than 1.25 billion, with half of them
in the sexually active age group. [2]
Among the 1000 studied cases, the majority were females i.e. 638 (63.8%)
while males were 362 (36.2%) in number, with a female to male ratio of
1.7:1. This is because a significant number of patients included in the
study (338) were from the RTI clinic of the Obstetrics and Gynaecology
department, where only female patients are registered. In patients
presenting to the STI clinic at the department of Dermatology, 362
(54.6%) were males and 300 (45.31%) were females, with a male to female
ratio of 1.2:1.
The majority of cases were in the 16-30 years age group i.e. 464
cases (46.4%), followed by 31-45 years age group i.e. 426 cases (42.6%),
which includes mostly sexually active individuals. Majority of cases
belonged to Punjab i.e. 905 (90.5%). Non residents of Punjab were 95
(9.5%) who came to Punjab from various states of India to earn their
daily living.
In our study, majority of patients i.e. 361 (36.1%) were educated up
to matric (tenth standard) including 236 (37.0%) females and 125 males
(34.5%), followed by 182 (18.2%) patients educated up to eighth standard
and 181 (18.1%) patients having education up to 12th standard. One
hundred and thirty six patients (13.6%) were educated up to primary
level, while 74 patients (7.4%) were illiterate. Sixty patients (6%)
were graduates while only 6 patients (0.6%) were post-graduates. Similar
findings were reported by Choudhry et al who observed that the majority
of the male patients attending STI clinics (53.12%) were educated up to
middle school while 50% of the females were illiterate. [3]
In another study by Choudhry et al, 67.64% patients were educated till
middle school while 26.47% were illiterate. [4]
Saikia et al reported that most patients in their study were from low
and middle income group and more than half (53.8%) had formal education.
[5] Setia et al also noted that most
patients presenting to the STI clinic were from middle to lower
socio-economic strata. [6]
In our study, out of 1000 patients, majority of patients i.e. 498
(49.8%) were housewives, followed by 154 (15.4%) patients who were daily
wagers, 84 patients (8.4%) private employees, 81 patients (8.1%)
farmers, and 73 patients (7.3%) were government employees.
In our study 904/1000 patients (90.4%) were married. Fifty-three
males (14.6%) and 14 females (2.2%) were un-married. Twenty-four females
(3.8%) were widows while 5 (0.8%) were divorcees. Similar findings were
reported by Choudhry et al, who observed that 70% patients in their
study were married. [3]
Setia et al reported that about 45% of the STI clinic attendees were
married, and this increased to 67% two years later in the course of the
study. Women attending the clinic were more likely to be married than
men. [6] Saikia et al reported that
45.7% having STIs were unmarried. [5]
In our study, 263 patients (27.3%) i.e. 235 males (64.9%) and 28
females (4.4%) had history of pre or extra marital sexual contact.
Similar to our study, Saikia et al reported among the married
individuals in their study, 68% admitted to having extra marital sexual
contact. [5] Setia et al reported that
males are more likely to admit to having multiple sexual partners than
females, due to the lower social standing of females in India. [6]
Choudhry et al observed that 31.3% patients in their study (all males)
had more than three sexual partners in the previous six months and 76.4%
had contact with commercial sex workers. [3]
In our study, the majority of female patients had bacterial vaginosis
i.e. 244 patients (38.2%), followed by 205 females (32.1%) having
candidial vulvovaginitis. Forty-seven females (7.4%) had cervicitis, 29
(4.5%) had herpes genitalis, 26 (4.1%) had ano-genital warts, 21 (3.3%)
had molluscum contagiosum while 12 females (1.9%) were diagnosed to have
pelvic inflammatory disease. Among the male patients, balanoposthitis
was most common, seen in 136 patients (37.6%), followed by herpes
genitalis in 91 (25.1%) patients, anogenital warts in 47 males (13.0%),
molluscum contagiosum in 28 (7.7%) patients.
Similar findings were reported by Choudhry et al, who observed that
33% males and 50% females presented with discharge. Also, 32% males and
27% females had genital ulcer. Other STIs seen were anogenital warts
(17%), umblicated nodules (5%). Multiple STIs were seen in 4% of the
patients. The majority of patients (28.7%) were diagnosed with Herpes
genitalis (HSV-2), followed by syphilis (23.7%), warts (20%), gonorrhoea
(19.3%) and Chlamydia (16.3%). HIV seropositivity was found in 10.3% of
the patients. Other STIs seen were T.vaginalis, molluscum contagiosum
and candidal balanoposthitis/vulvovaginitis. [4]
Saikia et al reported that out of 186 patients of STIs examined,
candidial vulvovaginitis in females and candidial balanoposthitis in
males were the most common STI (21.5%), followed by syphilis (17.2%),
genital warts (15%), herpes genitalis (11.3%), non-gonococcal urethritis
(10.8%), gonococcal urethritis (7%), pediculosis pubis (6.5%), chancroid
(5.9%) and lymphogranuloma venereum (4.8%). HIV seropositivity was found
to be 17.2 % in patients with STIs. [5]
The presence of one STI increases an individual's chance of acquiring
another STI. The presence of multiple STIs is a risk factor for
increased rate of transmission of HIV. The prevalence rate in Punjab is
0.32 % (Male- 0.37%; female- 0.26%). The positivity in various districts
of Punjab like Amritsa (4.49%), Tarn taran (3.07%), Gurdaspur (2.38%) is
high. [7] In our study, 124 patients
(12.4%) were found to be positive for HIV-1 antibodies while no patient
was found to be positive for HIV-2 antibodies.
Conclusion
Our study showed that the most common presenting complaint of the
patients was discharge per vaginum, with candidial vulvovaginitis being
the most common, followed by bacterial vaginosis. Viral STIs like herpes
genitalis and condylomata acuminata are on the rise among STI/RTI clinic
attendees.
References
1. Marfatia YS, Sharma A, Joshipura SP. Overview of
Sexually Transmitted Diseases. In: Valia RG, Valia AR, Editors. IADVL
Textbook of Dermatology. Mumbai, Bhilani Publishing House. 2010;1766-77.
2. National AIDS Control Organization. [homepage on
internet] NACO Annual Report 2011-12_ English [cited 2012 August 22];
Available from:
URL:http://www.nacoonline.org/Quick_Links/Publication/annual
_Report/NACO_Annual_Report/NACO_Annual_Report_2011-2012_English/.
3. Choudhry S, Ramachandran VG, Das S, Bhattacharya SN,
Mogha NS. Pattern of sexually transmitted infections and performance of
syndromic management against etiological diagnosis in patients attending
the sexually transmitted infections clinic of a tertiary care hospital,
Indian J sex Transm Dis, 31(2):104-8, 2010.
4. Choudhry S, Ramachandran VG, Das S, Bhattacharya SN,
Mogha NS. Characterization of patients with multiple sexually
transmitted infections: A hospital based survey, Indian J sex Transm
Dis, 31(2):87-91, 2010.
5. Saikia L, Nath R, Deuori T, Mahanta J. Sexually
transmitted diseases in Assam: an experience in a tertiary care referral
hospital, Indian J Dermatol Venereol Leprol, 75(3):329, 2009.
6. Setia MS, Jejrani HR, Brassad P, Boivin JF. Clinical
and demographic trends in a sexually transmitted infection clinic in
Mumbai (1994-206): An epidemiologic analysis, Indian J Dermatol Venereol
Leprol, 76;387-92, 2010.
7. Punjab State AIDS Control Society [homepage on
internet] Overview of HIV/AIDS in Punjab (Till July 2012) [cited 2012
August 22]; Available from:
URL:http://www.punjabsacs.org/OverViewHIV.aspx.
© 2013 Egyptian Dermatology Online Journal
|