|
|
Abstract
A 42 year old married male presented with a violaceous atrophic plaque
on the lower lip with bleeding on manipulation for the last 8 years. Biopsy
findings showed atrophic epidermis with effaced rete ridges and focal basal
cell layer degeneration with lymphocytic band in the dermis, with parakeratotic
horny pearls at places. Stratum corneum showed metaplastic changes. On the
basis of histopathology, a diagnosis of lichen planus (LP) with well differentiated
squamous cell carcinoma (SCC) was made. We are reporting this case as it
is rare presentation with mucosal LP of lower lip evolving into SCC.
Introduction
Lichen planus is a common dermatologic disorder involving the glabrous
skin, hair-bearing skin and scalp, nails, and mucous membranes of the oral
cavity, penis, and vulva. There have been multiple case reports of squamous
cell carcinoma developing within lesions of hypertrophic cutaneous lichen
planus and erosive oral lichen planus.
Case Report
A 42 year old male came with the complaint of a chronic, painful, non
healing ulcer on the muco-cutaneous junction of the lower lip since 8 years.
The patient had tried various topical and oral treatments with only partial
recovery and recurrence. The patient was a tobacco chewer and smoker since
20 years.
On examination, there was a violaceous plaque on the lower lip, with
well defined border and regular margins. An erosion was present in the centre.
On palpation, the border was not indurated. There was bleeding on manipulation.
There was no cervical or axillary lymphadenopathy. (Fig 1)
 | Fig 1:
Lesion on the lower lip, present for 8 years. |
|
Routine investigations were within normal limits. Skin biopsy was done,
which showed atrophic epidermis with effaced rete ridges and focal basal
cell layer degeneration with lymphocytic band in the dermis, with parakeratotic
keratin pearls at places. Stratum corneum showed metaplastic changes and
few atypical keratinocytes were seen in the sub-epidermal region. On the
basis of histopathology, a diagnosis of lichen planus with well differentiated
SCC was made. (Fig 2, 3)
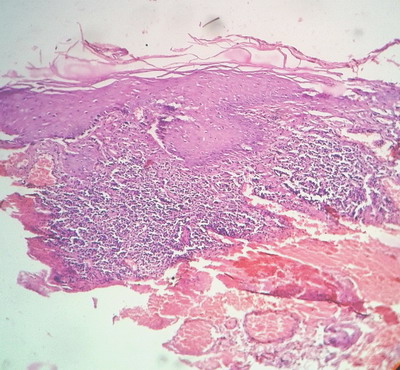
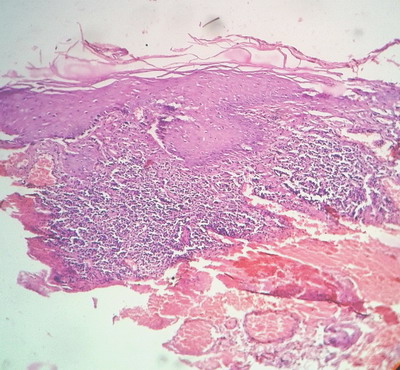 | Fig
2: Histopathology showing band like infiltrate at the
dermoepidermal junction and basal cell layer degeneration with
parakeratotic keratin pearls. |
|
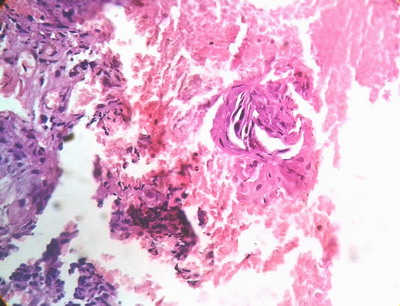
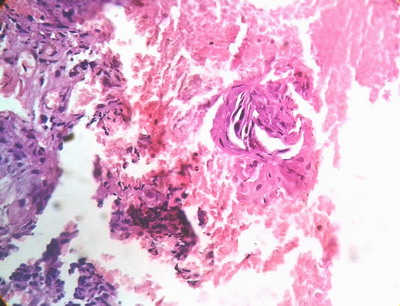 | Fig
3: Histopathology showing degenerated basal cells along with
keratin pearl. |
|
The patient was managed with surgical excision with flap rotation for
lip reconstruction. Histopathology revealed disease free margins.
Discussion
Oral lichen planus (OLP) is a chronic inflammatory mucocutaneous condition
which affects approximately 0.2% to 3.8% of the general population, being
more frequent in females.[1] The rate of
malignant transformation in OLP is about 0.4% to 1.74%.[2]
In a study conducted in 611 patients by Holmstrup et al, 9 patients (1.5%),
8 women (1.9%) and 1 man (0.5%) developed oral squamous cell carcinomas
(SCC) in areas of lichen planus lesions. OLP cases showed a 50-fold increase
in development of carcinoma as compared to age and sex matched controls
in the general population.[3]
Oral LP has an intrinsic property predisposing to neoplastic transformation.
Hence, it is necessary to follow-up the patients regularly at least annually
and possibly for life for the early diagnosis of a possible neoplastic degeneration.
These consideration are particularly important in the case of atrophic or
erosive OLP, and plaque OLP, especially when involving the dorsum of tongue.[4]
This highlights the importance of histopathology and role of serial biopsies
in early detection and timely management of SCC developing in OLP lesions.
References
1. Vincent SD, Fotos PG, Baker KA, Williams TP. Oral lichen
planus: The clinical, histological and therapeutic features of 100 cases.
Oral Surg Oral Med Oral Pathol 1990;70:165-71.
2. Van der Meij EH, Schepman PK, Van der Waal I. The possible
character of oral lichen planus and oral lichenoid lesions: A prospective
study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;96:164-71.
3. Holmstrup, P., Thorn, J. J., Rindum, J. and Pindborg,
J. J. (1988), Malignant development of lichen planus-affected oral mucosa.
Journal of Oral Pathology & Medicine, 17: 219-25.
4. Lo Muzio L, Mignogna MD, Favia G, Procaccini M, Testa
NF, Bucci E. The possible association between oral lichen planus and oral
squamous cell carcinoma: a clinical evaluation on 14 cases and a review
of the literature. Oral Oncology 1998, 34(4):239-46.
© 2014 Egyptian Dermatology Online Journal
|