|
|
Abstract
Pityriasis versicolor presents as scaly hyperpigmented or hypopigmented
macules on the chest, abdomen, back and proximal extremities. The atrophying
variant is very rare. We report a case of a 40 year old female who presented
with atrophic hyperpigmented and hypopigmented macules with fine scaling
all over the body with sparing of the face. The clinical differential diagnosis
considered were atrophying pityriasis versicolor, atrophoderma of Pasini
and Pierini, anetoderma, morphea, systemic lupus erythematosus and dermatomyositis.
Biopsy findings supported the diagnosis of atrophying pityriasis versicolor.
Introduction
Pityriasis versicolor is mild, chronic infection of the skin caused by
Malassezia yeasts, and characterized by discrete or confluent, scaly, discolored
or depigmented areas, mainly on the upper trunk. [1]
Atrophying pityriasis versicolor is a very rare variant characterized by
the presence of atrophy on the patches. This entity has been rarely reported
in the Indian literature.
Here we are reporting a rare case of atrophying pityriasis versicolor.
Case history
A 40 year old female presented to our department with hyper and hypopigmented
lesions all over the body since 3 years. The lesions initially began over
the abdomen and progressed over a span of 3 years to involve the chest,
back, upper and lower limbs with sparing of the face. The lesions were asymptomatic
without any itching or burning sensation. There was no history of application
of any medications over the lesions. Examination revealed multiple hyperpigmented
and hypopigmented macules with fine scaling and central atrophy over the
trunk, upper and lower limbs (Fig 1,2,3). Her systemic examination was
normal and there were no mucosal lesions.
 | Fig 1:
Multiple hyper and hypopigmented plaques with central atrophy on
abdomen |
|
 | Fig
2: Close up view showing atrophy |
|
 | Fig
3: Hypopigmented plaques on the back |
|
A differential diagnosis of atrophying pityriasis versicolor and lichen
sclerosis was made. A skin biopsy was performed from the atrophic hyperpigmented
macule over the abdomen. Biopsy showed few budding yeast forms in the superficial
layers of stratum corneum. Upper dermis showed sparse infiltrate of lymphocytes,
histiocytes and plasma cells (Fig 4). Periodic Acid Schiff (PAS) stain
showed numerous PAS positive spores of fungi (Fig 5,6).
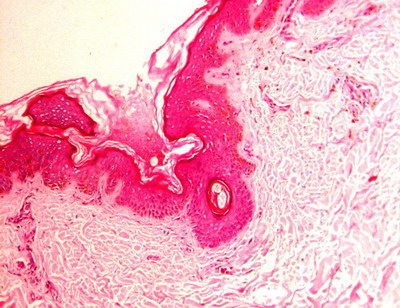
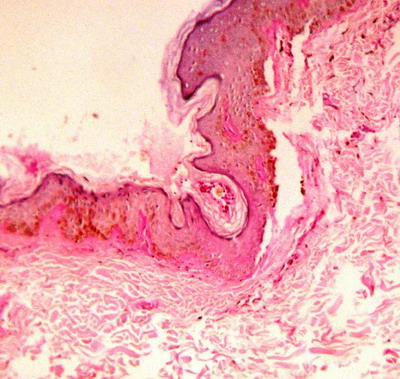
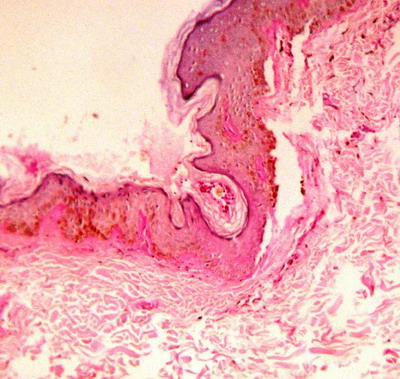
 | Fig
4: Histopathology revealing few budding yeast forms in the
superficial layers of stratum corneum. (H&E 40x) |
|
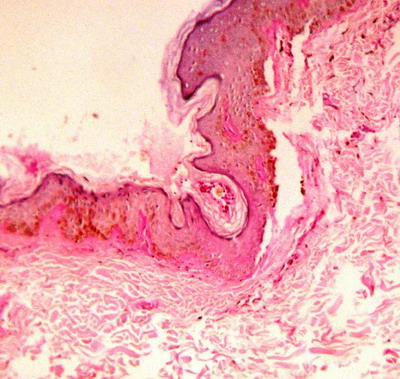
 | Fig
5: Periodic Acid Schiff (PAS) stain showing numerous PAS
positive yeasts and hyphal forms of fungi. (PAS stain 40x) |
|
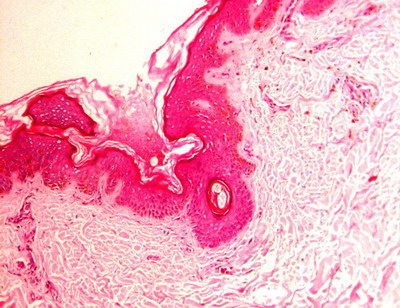
 | Fig
6: Close up view showing budding yeast forms. (PAS 100x) |
|
The patient was treated with a course of systemic and topical antifungals
and she was lost for the follow up.
Discussion
De Graciansky and Mery in 1971, first reported the skin atrophy on pityriasis
versicolor lesions. [2] Crowson and Magro
coined the term 'atrophying pityriasis versicolor'. [3]
Long term topical steroid use was believed to be a cause of atrophy in many
previous studies however, Crowson and Magro conducted clinical and histological
study on 12 patients of atrophying pityriasis versicolor, and found steroid
usage in only one patient. There was no usage of topical steroid in the
present case.
Crowson and Margo proposed that delayed type of hypersensitivity reaction
(DTH) may be operating in Pityrosporum spore colonization of skin. None
of their patients had eosinophils as a significant component of the infiltrate,
which implied a Th-1-dominant process, in which histiocyte recruitment and
activation by IFN- is a prominent feature. Histiocytes, like activated monocytes,
are a likely source of elastases and could explain the dermal elastolysis
noted in two of their patients. A Th-1-dominant immune reaction might contribute
to the epidermal atrophy through elaboration of tumor necrosis factor (TNF);
TNF-α causes apoptosis in keratinocytes and inhibits keratinocyte proliferation.
Low concentrations of pityrosporum organisms promote cytokine elaboration
like IL-1-β and TNF-α and high concentrations are inhibitory. This model
is consistent with that seen in epidermal colonization, where low numbers
of organisms are generally present on the skin surface. TNF-α inhibits
melanogenesis through the NF-κB pathway by down-regulating tyrosinase promoter
activity, thereby, it causes hypopigmentation.[3]
The clinical differential diagnosis considered were atrophoderma of Pasini
and Pierini, anetoderma, morphea, systemic lupus erythematosus and dermatomyositis.
However, histopathological reports were consistent with atrophying pityriasis
versicolor.
The prognosis of the disease is relatively good and the mycological recovery
and disappearance of atrophic lesions can achieved with systemic triazole
therapy or combined therapy of systemic triazole and topical imidazole.[4]
Many cases of atrophic pityriasis versicolor have been reported from
Korea.[4,5,6,7]
The case might be much more common than reported. Paucity of reports from
India may be due to under reporting or some cases going unrecognized. Atrophic
pityriasis versicolor should be included in the differential diagnosis of
atrophic skin lesions. Histology is diagnostic for these lesions.
References
1. Hay RJ, Ashbee HR. Mycology. In: Burns T, Breathnach
S, Cox N, Griffiths C, editors. Rook's textbook of dermatology. Oxford:
Wiley-Blackwell 2010; 36:10-36.13.
2. De Graciansky P, Mery F. Atrophie sur pityriasis versicolor
apres corticotherapie locale prolongee. Bull Soc Fr Dermatol Syphiligr.
1971; 78: 295.
3. Crowson AN, Magro CM. Atrophying tinea versicolor: a
clinical and histological study of 12 patients. Int J Dermatol. 2003; 42:
928- 932.
4. Park JS, Chae IS, Kim IY, Ko DK, Chung H, Lee SW. Achromatic
atrophic macules and patches of upper extremities. Indian J Dermatol Venereol
Leprol 2013; 79: 270.
5. Yang YS, Shin MK, Haw CR. Atrophying Pityriasis Versicolor:
Is This a New Variant of Pityriasis Versicolor? Ann Dermatol 2010; 22: 456-459.
6. Lee DB, Chae WS, Jung HN, Choi YS, Suh HS. A Case of
Pityriasis Versicolor Atrophicans. Korean J Med Mycol 2012; 17: 47-50.
7. Noh TW, Hong KC, Kang YS, Lee UH, Park HS.Atrophying
Pityriasis Versicolor. Korean J Dermatol 2012; 50: 447-450.
© 2014 Egyptian Dermatology Online Journal
|