|
|
Abstract
A 36-year-old female presented with cone-shaped skin lesions on the scalp
and retro-auricular area of 7 months' duration. Histopathological findings
showed dense inflammatory cell infiltration and remarkable Munro's microabscesses
in the horny layer in addition to psoriasiform epidermal hyperplasia, and
predominant dermal edema. Based on clinicopathological findings, a diagnosis
of psoriasis rupioides capitis was made. She was initially treated with
oral methotrexate 15 mg weekly and topical clobetasol-salisylic acid ointment
and coal tar ointment for three months with no response. Then she was put
on acitretin 25 mg oral daily on which she was improved.
Introduction
Rupioid psoriasis is characterized by very thick rock like convex lesions.
It is also called ostraceous psoriasis. It is relatively resistant to topical
treatment due to thick scaly barrier which prevents the absorption of topical
drugs. Rupioid psoriasis is associated with chronic plaque psoriasis or
psoriatic arthropathy in most of the reported cases. I am presenting an
isolated case of psoriasis rupiodes capitis which responded to oral acitretin.
Case Report
A 36-year-old female presented with limpet-like, cone shaped skin lesions
with mild erythema on the scalp and retro-auricular area for the last 7
months. On history, she developed a small pea size red scaly nodule on scalp
which later on enlarged and became hard. There was no history of joint pains,
burning micturation or orogenital ulceration. There was also no history
of photo-aggravation of the lesions or photosensitivity.
On examination, the lesions were present on the scalp and retro-auricular
area. The lesion on the scalp was about 5cm in size, oval in shape with
convex surface and yellow in color. The lesions of retro-auricular area
were two to three in number on each side and their sizes varied from 1-2
cm. All the lesions were rock hard and non-tender. There was no cervical
lymphadenopathy and nails were normal.

| Fig 1: Rock hard cone shaped elevated
lesion of Rupioid psoriasis on scalp |
|

| Fig 2: Lesions of Rupioid psoriasis in
retroauricular area |
|
On blood investigations, all the parameters were normal including the
ESR, C-reactive protein and RA factor. The serological tests for syphilis,
HIV and Hepatitis B were negative. Urine examination was normal. KOH mount
of plucked hair and scrapings of lesions was done and was negative and culture
for fungal elements was negative.
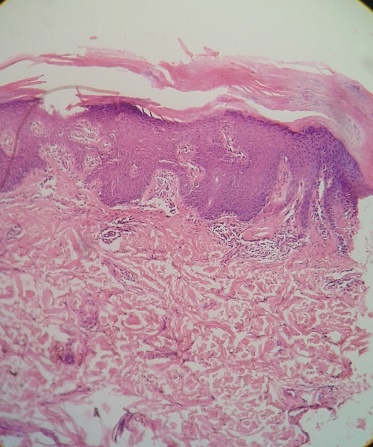
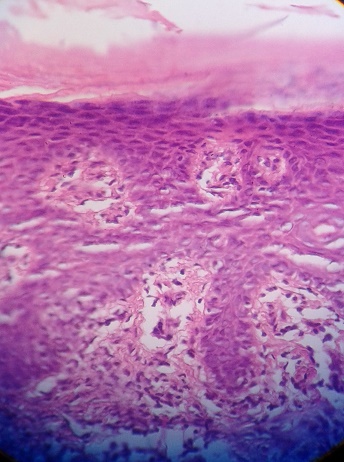
Incisional biopsy was done from the margin of the lesion on the scalp
which showed psoriasiform epidermal hyperplasia with marked Munro's microabscesses
in the horny layer and in the dermis, dense inflammatory cell infiltration
and no granuloma or malignant cells.
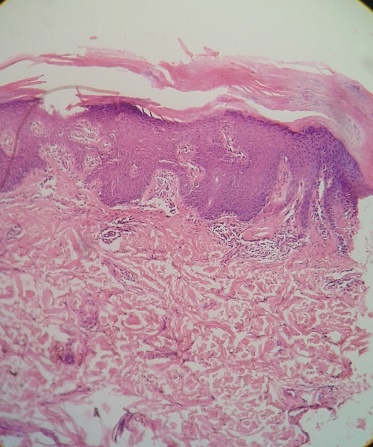
| Fig 3: Histopathology (10X view-H&E
stain) of scalp lesion showing marked epidermal
hyperplasia |
|
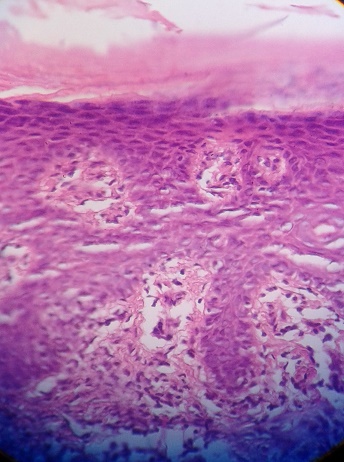
| Fig 4: Histopathology (40X view-H&E
stain) of scalp lesion showing Munro's
microabscesses. |
|
Overall, on the basis of the clinical and histological findings the diagnosis
of psoriasis rupioides capitis was made.
She was initially put on oral methotrexate 15mg weekly and topical clobetasol-salisylic
acid ointment for three months under occlusion and coal tar ointment at
night, but no improvement was seen. Then she was shifted to oral acitretin
25 mg daily and improvement started in the form of reduction in size of
the lesions over 2 weeks.
Discussion
Psoriasis is a common inflammatory disease of the skin and joints. It's
cause remains unknown; however, it has been linked to complex interactions
between predisposing genes and the environment. The pathophysiology of psoriasis
is characterized by epidermal hyper-proliferation, enhanced antigen presentation,
helper T cell (Th1) and Th17 cytokine production, T cell expansion and angiogenesis.[1]
Only a few cases have been reported involving a rare variant of rupioid
psoriasis with cone-shaped, limpet-like lesions.[2,3,4,5]
Rupioid skin lesions have also been observed in Reiter's disease and secondary
syphilis.[6,7]
Although the pathogenesis of rupioid lesions remains unclear, the aberrant
keratinization in combination with the inflammatory process followed by
the voluminous sero-exudate is likely to create the hard rupioid lesions.[8]
The concept behind using the acitretin in rupioid psoriasis is that acitretin
normalizes epidermal cell proliferation, differentiation and cornification.[9,10]
It is thought to exert these effects by interfering with the expression
of epidermal growth factor genes. Acitretin is licensed for use in severe
extensive psoriasis which is resistant to other forms of therapy, including
topical, light and systemic.
Acknowledgement
My special thanks to Dr. Rashmi Gupta consultant "PEARL- THE SKIN & COSMETIC
CLINIC" for her support in manuscript preperation.
References
1. Gupta SK, Singh KK, Lalit M. Comparative therapeutic
evaluation of different topicals and narrow band ultraviolet B therapy combined
with systemic methotrexate in the treatment of palmoplantar psoriasis. Indian
J Dermatol 2011;56:157-62.
2. Camp RDR. Psoriasis. In: Rook A, Wilkinson DS, Ebling
FJG, eds. Textbook of Dermatology, 5th edn, Vol 3. Oxford: Blackwell Science
Ltd, 1992: 1391-457.
3. Cvejic S, Milakov J. Psoriasis rupioides et verrucosa.
Med Pregled 1967; 20: 67-179.
4. Golousenko II, Fadeeva VI, Omran A. Case of psoriasis
rupioides with arthropathy. Vestnik Dermatologii I Venereologii 1984; 3:
74-5.
5. Wang J-L, Yang T-H. Rupioid psoriasis associated with
arthropathy. J Dermatol 1997; 24: 46-9.
6. Sehgal VN, Koranne RV, Shyam PAL. Unusual manifestations
of Reiter's disease in a child. Dermatologia 1985; 170: 77-99.
7. Held JE, Ross M, Beltrani V Jr. et al. Noduloulcerative
or `malignant' syphilis occurring in an otherwise healthy woman: Report
and review of dramatic dermatosis. Cutis 1990; 45: 119-22.
8. T. Murakami, M. Ohtsuki and H. Nakagawa. Rupioid psoriasis
with arthropathy. Clinical and Experimental Dermatology, 2000; 25(5): 409-12.
9. Tong PS, Horowitz NN, Wheeler LA. Trans retinoic acid
enhances the growth response of epidermal keratinocytes to epidermal growth
factor and transforming growth factor beta. J Invest Dermatol 1990; 94:
126-31.
10. Zheng ZS, Polakowska R, Johnson A et al. Transcriptional
control of epidermal growth factor receptor by retinoic acid. Cell Growth
Differ 1992; 3: 225-32.© 2014 Egyptian
Dermatology Online Journal
|