|
|
Summary
A 40-year-old male presented with itchy small nodules over the thigh,
scrotum and pubic area of gradual onset and progressive course of 9 months
duration. Histopathologic examination revealed horn filled crater with lip
like projection at the side of the crater.
Introduction
Keratoacanthoma (KA) is a relatively common low-grade malignancy that
originates in the pilosebaceous glands and pathologically resembles squamous
cell carcinoma (SCC). In fact, strong arguments support classifying KA as
a variant of invasive SCC [1]. In most pathology/biopsy reports, dermatopathologists
refer to the lesion as "squamous cell carcinoma, keratoacanthoma-type".
KA is characterized by rapid growth over a few weeks to months, followed
by spontaneous resolution over 4-6 months in most cases. KA reportedly progresses,
although rarely, to invasive or metastatic carcinoma; therefore, aggressive
surgical treatment often is advocated. Whether these cases were SCC or KA,
the reports highlight the difficulty of distinctly classifying individual
cases [2, 3, 4, and
5].
Case Presentation
A 40-year-old-male, working as a car mechanic, presented with itchy small
nodules over the groin area of gradual onset and progressive course of 9
months duration. On examination, there were multiple pinkish-red dome-shaped
firm nodules which were sharply marginated with raised borders and measuring
0.5 to 1mm. The closer inspection of the lesions revealed smooth crater
filled with central keratin plug that was projecting like a horn on the
smooth shiny surface of the nodules which were localized to the skin of
the thigh, scrotum and pubic area.
 | Fig 1:
multiple pinkish-red dome-shaped firm well defined nodules
affecting the scrotum and groin |
|
 | Fig
2: The well-defined nodules show a smooth crater filled with
central keratin plug. |
|
Differential diagnosis included: giant warts, multiple keratoacanthoma,
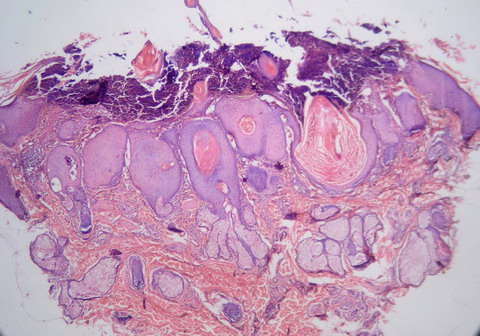
prurigo nodularis and squamous cell carcinoma. Histopathologic examination
revealed horn like crater surrounded by lip like projection and the strands
of the epidermis were protruding in to the dermis. Those findings were consistent
with diagnosis of multiple keratoacanthoma.
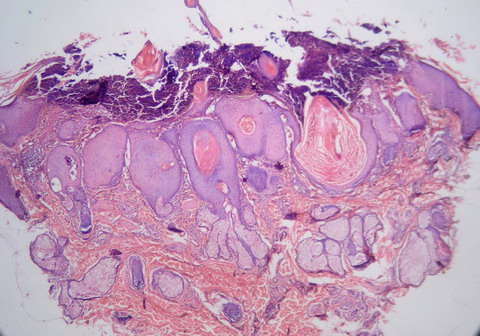 | Fig
3: H&E stained specimen form the groin lesions showing horn
like crater surrounded by lip like projection and the strands of
the epidermis were protruding in to the dermis (10x) |
|
Discussion
Keratoacanthoma (KA) typically grows rapidly, attaining 1-2 cm within
weeks, followed by a slow involution period lasting up to 1 year and leaving
a residual scar if not excised preemptively. Since expedient therapy almost
always is instituted, the true natural course of the tumor cannot be confirmed
with certainty.
Physical findings in KA are limited to the skin. The lesions typically
are solitary beginning as firm, roundish, skin-colored or reddish papules
that rapidly progress to dome-shaped nodules with a smooth shiny surface
and central crateriform ulceration or keratin plug that may project like
a horn. Most keratoacanthomas occur on sun-exposed areas. The face, neck,
and dorsum of the upper extremities are common sites, while truncal lesions
are rare.
Both sunlight and chemical carcinogens have been implicated as pathological
factors in growth of the tumor. Trauma, human papilloma virus, genetic factors,
and immunocompromised status also have been implicated as etiologic factors.
In this case, the patient being a car mechanic exposed to tar and trauma,
the lesions developed in hidden areas of the body other than sun exposed
ones.
KA is less common in darker-skinned individuals, rarely affects persons
less than 20 years, the incidence increases with age and male-to-female
ratio for is 2:1. It may be a component of Muir-Torre syndrome, which is
a cancer-associated genodermatosis with multiple sebaceous neoplasms (adenomas,
epitheliomas, carcinomas, Keratoacanthomas), and gastrointestinal malignancies
(most commonly colon), although other carcinomas have been reported (genitourinary,
pulmonary, endometrial). When Muir-Torre syndrome is diagnosed, an age-appropriate
cancer screening workup is indicated. An approximately equal number of internal
malignancies are diagnosed before and after the cutaneous neoplasm. These
internal malignancies tend to be low grade, but early diagnosis is important.
Colonoscopy, rather than flexible sigmoidoscopy, is recommended, since the
colon cancer frequently is found in the right ascending colon, proximal
to the hepatic flexure.
KA is believed to have a good prognosis; however, it has been reclassified
as SCC-KA type to reflect the difficulty in histological differentiation,
as well as the uncommon but potentially aggressive nature of KA. It infrequently
presents as multiple tumors and may enlarge (5-15 cm), become aggressive
locally, or rarely, metastasize [6, 7].
The treatment includes surgical excision (primary intervention), radiotherapy
and medical treatment using systemic steroids, systemic retinoids, intralesional
methotrexate, 5-fluorouracil and bleomycin.
References
1. Manstein CH, Frauenhoffer CJ, Besden JE. Keratoacanthoma:
is it a real entity? Ann Plast Surg. 1998; 40 :469-72.
2. Schwartz RA. Keratoacanthoma. J Am Acad Dermatol. 1994;
30: 1-19.
3. Magalh„es RF, Cruvinel GT, Cintra GF, Cintra ML, Ismael
AP, de Moraes AM. Diagnosis and follow-up of keratoacanthoma-like lesions:
clinical-histologic study of 43 cases. J Cutan Med Surg. 2008; 12: 163-73.
4. Kossard S, Tan KB, Choy C. Keratoacanthoma and infundibulocystic
squamous cell carcinoma. Am J Dermatopathol. 2008; 30: 127-34.
5. Cribier B, Asch P, Grosshans E. Differentiating squamous
cell carcinoma from keratoacanthoma using histopathological criteria. Is
it possible? A study of 296 cases. Dermatology. 1999; 199 :208-12.
6. Frank TL, Maguire HC Jr, Greenbaum SS. Multiple painful
keratoacanthomas. Int J Dermatol. 1996; 35: 648-50.
7. Sanders S, Busam KJ, Halpern AC, Nehal KS. Intralesional
corticosteroid treatment of multiple eruptive keratoacanthomas: case report
and review of a controversial therapy. Dermatol Surg. 2002; 28: 954-8.
© 2014 Egyptian Dermatology Online Journal
|