|
|
Abstract
Cheilitis granulomatosa is characterized by recurrent or persistent
swelling of one or both lips. The exact etiology is not certain. It may
represent oral manifestations of Crohn's disease and sarcoidosis, so the
complete diagnostic work up of the patient with suspected Cheilitis
granulomatosa is a must. Microscopically, a non-necrotizing granulomatous
inflammation is the typical feature. Management depends upon the severity of
the condition and the patient's esthetic concerns. Here a case of
successfully treated Cheilitis Granulomatosa along with gingival involvement
in an 18 year old female is presented along with its clinical features.
Keywords: cheilitis; female; granuloma; Intralesional steroid
Introduction
Cheilitis Granulomatosa (CG) is a rare granulomatous disease of uncertain
etiology, described by German dermatologist Miescher in 1945 as a distinct
clinicopathological entity, characterized by diffuse, not tender, soft to
firm recurrent or persistent swelling of one or both lips. [1]
CG has often been associated with other orofacial Granulomatous disorders
e.g. atypical Tuberculosis, Anderson-Fabry disease, Crohn's disease,
sarcoidosis, and allergic reaction. It is also considered as an
oligo-symptomatic or mono-symptomatic form of Melkersson Rosenthal syndrome
(MRS). CG usually affects young adults, mostly in the 2nd decade of life
with a female predominance with incidence of 0.08% [1].
The diagnosis of cheilitis granulomatosa is made by correlation of the
patient's history and clinical features, supported by the histopathological
findings. Management of cheilitis granulomatosa is difficult, as described
in the literature. Different treatment modalities have been reported, from
various conservative treatments to surgical interventions, with variable
outcome. [2] Case Report
An 18 year old female patient reported with a chief complaint of swelling
in upper lip and anterior gums since last 5 years, which was painless and
persistent. History of the presenting illness revealed that initially there
was a swelling of the upper lip followed by the anterior gum and slowly
progressed to the present extent, with exacerbation and remission periods
since 3 years. There was no apparent history of trauma, allergy to any
substance, insect bite, pain in the teeth, pus discharge, fever, facial
paralysis or any other history of systemic ailment. Patient consulted a
physician 2 months back for the same problem, and was prescribed symptomatic
systemic medication, but got no relief. Patient was unaware about the
medication prescribed as the records were not available. The family history
and past dental history of the patient were non-contributory. The swelling
was consistent in size without any aggravating or relieving factors. On
general physical examination, the patient appeared moderately built and
nourished with the other vital signs were within the normal limits. Extra
oral examination revealed a diffuse swelling of upper lip with smooth and
intact overlying skin, with dry and scaling of upper lip. On palpation, the
lip swelling was soft in consistency, non-tender, non-fluctuant and there
was no localized increased in the temperature. Regional lymph nodes were not
palpable. Intraoral examination revealed midline crack and bleeding spot in
the upper lip. In upper anterior region, the gingiva was lobulated and
enlarged, extending mesio-distally from upper right canine to left canine
regions and superior-inferiorly from labial vestibule to partially covering
the crowns with blunting and enlargement of interdental papillae. In the
lower anterior region, gingiva was enlarged from left canine to right canine
region, with apparent inflammation. Enlarged gingiva was reddish pink in
color, soft to firm, with loss of stippling & bleeding on probing. [Fig.1]
 | Fig 1:
Extra orally, diffusely enlarged upper lip which was soft,
non-tender with smooth and intact overlying skin. Intra-orally,
there was midline crack and bleeding spot visible. Also, the
anterior gingiva inflamed, red, soft to firm and with bleeding on
probing. |
|
On the basis of history and clinical examination, a provisional
diagnosis of Chronic Idiopathic Granulomatous lesion of the upper lip and
gingiva was made. The differential diagnosis included cheilitis
granulomatosa, angioedema, cheilitis glandularis, neurofibroma, exfoliative
cheilitis, plasma cell cheilitis, sarcoidosis, Crohn's disease, and
tuberculosis. Vitality test in relation to involved teeth region was done
and teeth were found to be vital. Routine Blood investigations (Hb%, BT, CT,
TLC, DLC), RBS, HbSAg and HIV were in the normal range except there was
increased ESR. On endoscopic examination to rule out Crohn's disease, the
intestinal mucosa appeared normal. The chest radiograph appeared normal.
Patch testing was done for commonly used food products and cosmetics and the
results were negative. An incisional biopsy of the lip and gingiva was
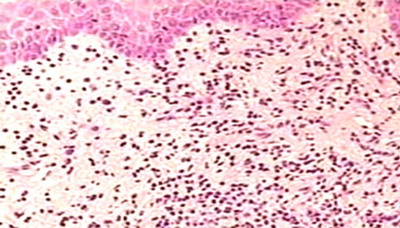
performed under local anesthesia. Biopsy specimen revealed stratified
squamous parakeratinized epithelium overlying an edematous connective tissue
stroma with areas of noncaseating granulomatous infiltrate consisting of
lymphocytes, foamy histiocytes, epitheloid cells and multinucleated giant
cells, which were suggestive of chronic granulomatous lesion of the lip
[Fig.2].
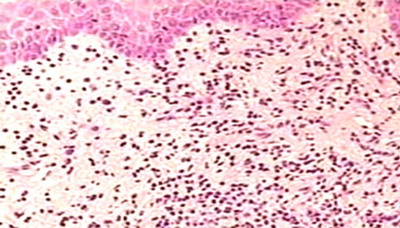 | Fig
2: Photomicrograph of the lesion showing infiltrates of
inflammatory cells in sub epithelial connective tissue. (H & E,
x40). |
|
Based upon the history, clinical examination and subsequent
investigations, a final diagnosis of Cheilitis granulomatosa of the upper
lip and anterior gingiva was made. Treatment included intralesional
injections of 0.1ml of Triamcinolone Acetonide (TA) (40 mg/mL) into the
upper lip vermillion and mucosa and anterior gingiva after mixing 0.05ml of
adrenaline in the injection, on weekly bases for 2 months. There was a
significant reduction in the lip and gingival swelling. The swelling
regressed following our treatment and the patient was asymptomatic after
treatment. [Fig.3]. The patient was re-evaluated each week for the
next 6 weeks for any recurrence. Subsequently, the patient is under follow
up since 18 months and has shown no signs of recurrence.
 | Fig
3: Showing reduction in the swelling of upper lip and anterior
gingiva. |
|
Discussion
The exact etiology & pathogenesis of CG is unknown. Hornstein suggested
that the CG may be caused by an alteration in autonomic nervous system
function localized to facial skin, resulting in increased vascular
permeability and edema.[1] Other etiologic
factor documented is cell mediated hypersensitivity reaction as there is
presence of activated helper T lymphocytes expressing interleukin-2
receptors in these lesions.[3] It is also
postulated that the cytokine production by lymphocytic clone could be
responsible for the formation of granulomas in CG.[4]
Chronic focal infections, sensitivity to food items and lymphatic vessels
obstruction have been suggested as contributing factors.[1]
According to Kano et al.,[5] some patients
with CG are predisposed to Crohn's disease, and CG may precede intestinal
Crohn's disease by few years. Worsaae and Pindborg reported that gingival
swelling may precede the lip swelling and the gingival manifestations
appeared mainly in the anterior part of the mouth.[6].
In the present case gingival enlargement preceded the lip swelling. In our
case CG occurred on the upper lip which was in accordance to the available
literature which stated that upper lip was the most common site of
occurrence. Histologically, there is dilation of lymphatic vessels,
perivascular lymphocytic infiltration and to a varying degree
non-necrotizing granulomas are seen in the lamina propria. Typically, the
granulomas appear to cluster around scattered vessels and are not well
formed or discrete. Fibrosis may be present in long term lesions.[1]
Diagnosis of CG is done by ruling out other conditions. The differential
diagnosis for a swollen lip can be extensive but a good clinical history and
thorough clinical examination will usually eliminate many diagnostic
possibilities.[7] In approximately 42% of
MRS patients, CG precedes other signs but reverse is not true as most of CG
patients never develop MRS. Van der Waal et al., state that, although
non-caseating granulomas are classically present, the histology may be
nonspecific, with edema and perivascular lymphocytic infiltrate.[8]
The diagnosis of CG is therefore a diagnosis of exclusion. It is necessary
to exclude the possible local and systemic diseases that can have similar
clinical manifestations, including hypersensitivity reactions. Further
workup includes sarcoidosis, Crohn's disease, tuberculosis, deep fungal
infections, leprosy, leukemic infiltrate, and foreign body reactions.
Sarcoidosis is unlikely in the absence of respiratory problems, and if chest
x-ray and ACE levels are normal. Biopsy of labial salivary gland can be of
help in diagnosing sarcoidosis. Crohn's diseases can be ruled out if
gastrointestinal complaints are absent.[9]
IgE levels and patch test may be of diagnostic value when hypersensitivity
reaction is suspected. Tuberculosis should be ruled out by acid fast
bacillus staining and chest radiographs.[10]
Management of CG is dependent on correct diagnosis of the condition and
identification of any precipitating factors. Patients without dental
infections with CG should be enquired for the presence of systemic signs and
symptoms of Crohn's disease, sarcoidosis or a history of angioedema. In the
presence of positive findings, the patient should be referred for further
systemic evaluation. Various documented treatment modalities includes
surgery, oral and intralesional Corticosteroids and boiled water injections,
drugs like antituberculous drugs, antibiotics, vitamins, phenylbutazone,
ACTH.[1] Corticosteroids have been shown to
be effective in reducing lip swelling and preventing recurrences and are
considered the mainstay of therapy. Patient with mild swelling can be
managed by using topical steroids. Severe cases of swelling of the lip can
be treated with Intralesional Triamcinolone Acetonide (0.1%) injections.
Patients with more extensive lip swelling can be initially treated with
systemic medication.[11] Surgery is
indicated only in severely disfiguring cheilitis and once the disease has
been brought into a quiescent phase and should thereafter be treated with
biweekly to monthly Triamcinolone 0.1% injections for 2-6 months to prevent
relapse.[12] Recurrence, though minor, is
not uncommon. Therefore, treatment is currently mainly empirical, and based
largely on the severity of symptoms. In our patient the intralesional
Triamcinolone resulted in resolution of the lesion with no recurrence during
the follow up period. Surgical re-contouring is not frequently used as there
is an increased risk of recurrence. Prognosis is variable and is best in
early diagnosed cases.[13]
References
1. Ceena DE, Ashok L, Shivprasad S,
Anitha B, Ahmed Mujib BR. Cheilitis granulomatosa. Journal of Indian Academy
of Oral Medicine and Radiology.2006; 18: 167-9.
2.
Burton JL, Scully C. Textbook of Dermatology, Vol. 4, 6th edi. Oxford:
Blackwell Science, 1998: 3139-41.
3. Shams MG,
Motamedi MH, Azizi T. Orofacial granulomatosis of the lower lip and cheek:
report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;
104:e42-4.
4. De Quatrebarbes J, Cordel N, Bravard P,
Lenormand B, Joly P. Miescher's cheilitis and lymphocytic clonal expansion:
2 cases. Ann Dermatol Venereol. 2004; 131:55-7.
5.
Kano Y, Shiohara T, Yagita A, Nagashima M. Association between cheilitis
granulomatosa and Crohn's disease. J Am Acad Dermatol 1993; 28: 801.
6. Worsaae N, Pindborg JJ. Granulomatous gingival manifestations of
Melkersson-Rosenthal Syndrome. Oral Surg Oral Med Oral Pathol 1980; 49:
131-8.
7. El-Hakim M, Chauvin P. Orofacial
granulomatosis presenting as persistent lip swelling: review of 6 new cases.
J Oral Maxillofac Surg 2004; 62: 1114-7.
8. van der
Waal RI, Schulten EA, van der Meij EH, van de Scheur MR, Starink TM, van der
Waal I. Cheilitis granulomatosa: overview of 13 patients with long term
follow up- results of management. Int J Dermatol. 2002; 41: 225-9.
9. Bellil K, Chelly I, Ben Ghorbel I, Mekin A, Bellil S, Kehir N, et al.
Salivary gland biopsy:experience of La Rabta Hospital's pathology
department. Tunis Med 2007; 85: 64-6.
10. Mignogna
MD, Fedele S, Lo Russo L, Lo Muzio L. Orofacial granulomatosis with gingival
onset. J Clin Periodontol. 2001; 28:692-6.
11. Grave
B, McCullough M, Wiesenfeld D. Orofacial granulomatosis: a 20 year reviews.
Oral Dis 2009; 15: 46-51.
12. Krutchkoff D, James R.
Cheilitis granulomatosa: Successful treatment with combined local
triamcinolone injections and surgery. Arch Dermatol 1978;114:1203-6
13. Wiesenfeld D, Ferguson MM, Mitchell DN, MacDonald DG, Scully C, Cochran
K, et al. Oro-facial granulomatosis-a clinical and pathological analysis. Q
J Med. 1985; 54:101-13.© 2015 Egyptian
Dermatology Online Journal |