|
|
Abstract
Holi is a festival of colours, traditionally celebrated by greeting
others and applying various colours. These colours are synthetic dyes which
may have harmful side-effects on the skin and mucocutaneous areas like the
conjunctiva and oral mucosa. In India, these colours are prepared on a small
scale and lack any quality checks. Here we present a case of a 43 years old
female who developed angioedema with urticaria progressing into urticarial
vasculitis after playing with the colours in the festival of Holi. This case
report highlights the need to put manufacturing of Holi colours under the
guidelines of the Food and Drug Cosmetic Act and the Bureau of Indian
Standards Key words: Holi colours, female, angioedema, urticarial
vasculitis. Introduction
Cultural and religious practices may have significant impact on the
health of people.Holi, an annual festival celebrated all over India since
ancient times is one of the most popular annual events in India, observed
with great festivity. On this day people gather together in a common place
and celebrate this festival by applying colours in different forms on
friends and family. Originally, the bright flowers that blossomed during
spring were used as raw materials from which the different shades of Holi
colours were made. Most of these trees were supposed to have medicinal
properties beneficial to the skin. Lately with the spread of
industrialization and urbanization, natural colours have been replaced by
inexpensive industrial dyes manufactured through different chemical
processes. Many patients consult dermatologists over the few days
immediately following Holi for skin problems resulting from playing with
these colours. Case report
A 43 years old female presented with chief complaints of the swelling
over the face, eyes and multiple red coloured lesions all over the body,
associated with itching and burning sensation. She gave a history of playing
with colours on her body which enterd her eyes and oral cavity followed by
the appearance of these lesions on the very next day. These lesions were
gradually progressive in nature. She had a past history of similar episode
in the form of generalised pruritus after exposure to the Holi colours. She
gave no history of any drug intake, hair dye application, atopic diathesis,
local irritant application, joint pains, dyspnoea, fever, chest pain or
vomiting. On examination there were multiple erythematous urticarial
wheals and papules. Plaques were of varying sizes ranging from 0.3x0.5 cm
and 1x1 cm to 1x3 cm and 2x4 cm over the face, both upper and lower limbs,
back, chest, abdomen, thighs, legs and buttocks (Fig. 1).There was
oedema of facial skin with angioedema of the upper lip and eyes with
congestion and watering of both eyes (Fig. 1).
 | Fig 1:
Erythematous urticarial wheals, papules, plaques of the face and
neck with congestion and angioedema of right eye and upper lip. |
|
Lesions present on the thighs, back, abdomen were purpuric and non-tender
(Fig. 2). Further these lesions progressed over both palms and soles.
The patient also developed congestion and erosions of the oral mucosa. Her
systemic examination revealed no abnormality.
 | Fig
2: Multiple purpuric patches of both thighs and legs
posteriorly. |
|
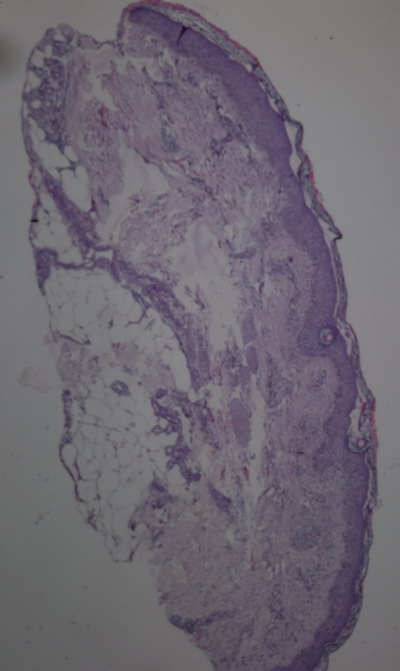
The
complete blood counts were normal. Eosinophil count was 4% with absolute
eosinophil count of 392 cells/mm≥). Blood sugar, renal and liver profile
were within normal limits. ELISA for HIV was non reactive and RA factor,
Antinuclear antibodies (ANA) level and thyroid profile were normal. Skin
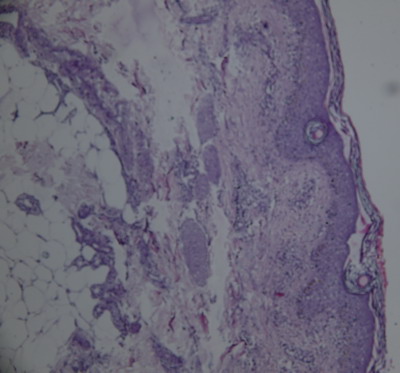
biopsy revealed urticarial vasculitis showing dermal oedema with
perivascular infiltrate consisting of inflammatory cells in the dermis
(Fig. 3&4).
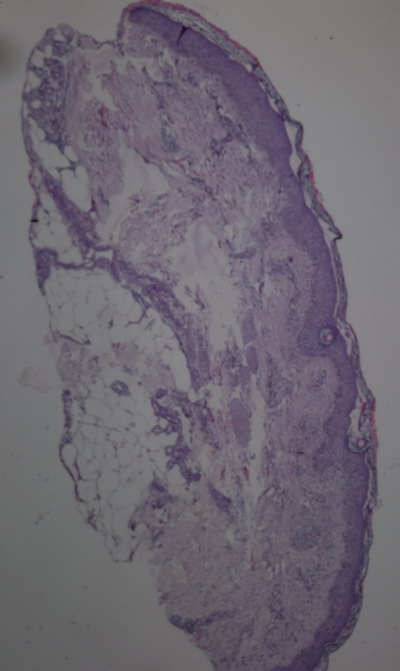 | Fig
3: Photomicrograph of urticarial vasculitis showing inflammatory
cells around the dermal vessels (H&Ex400). |
|
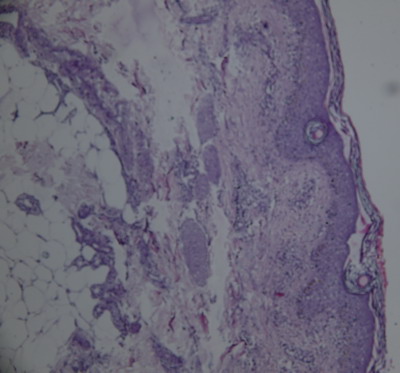 | Fig
4: Photomicrograph of urticarial vasculitis showing dermal
oedema with perivascular inflammatory cells (H&E). |
|
The patient
was treated with intravenous dexamethasone 8 mg a day over two days which
was tapered reducing the dose 8 mg daily for two days. It was then followed
by shifting to tablet Prednisolone 20mg which was tapered over two days by
reducing the dose to 10 mg and was then stopped. Her blood sugar level was
also monitored while she was on steroids and it remained normal. The patient
was also given injectable and oral antihistamines with local care for the
eyes and oral mucosa. She was completely asymptomatic after three days of
treatment. Fig.5&6 show complete resolution of facial and ocular
lesions with clearance of purpuric lesions of thighs and legs.
 | Fig
5: Post-treatment photograph showing complete clearance of
lesions of face and eyes. |
|
 | Fig
6: Post-treatment photograph showing complete resolution of
purpuric patches of the thighs and legs on posterior aspect. |
|
Discussion
Religious activities are involved in the celebration and the ritual of
Holi involves throwing of various forms of colours on one another. The
colours used during the festival come in different forms including pastes,
coloured powders and watercolours. The colours mainly include synthetic dyes
like malachite green, auramine, methyl violet, rhodamine and orange II. Some
of the commonly used colours and their ingredients are black (lead oxide),
green (copper sulfate and malachite green), silver (aluminium bromide), blue
(Prussian blue), and red (mercury sulfate).The dry colours, commonly known
as 'gulals' or 'abeer', have two components; a colourant and a base, both of
which may cause cutaneous problems. Mica dust which is often added as a
sparkling agent to the dry powders, can lead to multiple micro- traumas of
skin and predisposition to infections. The use of contaminated starch or
wheat flour can further increase the chances of skin or ocular infections.
Most of these chemicals are phototoxic and may incite skin allergies. Dada
et al [1] have reported ocular injuries due
to Holi colours. In another case report, the patient suffered from bilateral
periorbital necrotizing fasciitis, following exposure to Holi colours [1].
Periorbital necrotizing fasciitis carries a high rate of mortality of up to
12.5% [1]. According to a study, malachite
green was the main component of the Holi colours used that caused the severe
ocular irritation with epithelial defect upon exposure [2].
According to a study, skin problems occured quite frequently following the
celebration with colours, in which approximately 54.1% of the patients
complained of pruritus, burning sensation and eczematous reaction pattern as
the commonest clinical findings [3]. There
is paucity of data with respect to these incidences and enough data were not
available to support our findings. In our case report the skin as well as
mucosal involvement in the form of angioedema with urticaria were the main
clinical features and the presentation as urticarial vasculitis in itself is
a rarity. A limitation of this case report has been the inability to perform
an appropriate patch test to detect the precise etiology because the
colorants were not available with the patient at the time of presentation
and the reactions could have been due to unknown industrial dyes. The
patient was also apprehensive for the test as she had the fear of
aggravation of lesions on contact with the chemical. Holi colours are
produced in India without any quality checks and are sold freely in the
market. Packets of these colours do not provide any information to the
consumer about the source of the colours, contents, and side effects.
Several non-governmental organizations have started campaigning for safe
practices like colours derived from natural sources such as vegetables and
flowers as colours in Holi. We believe that extensive efforts to increase
public awareness regarding the health hazards of harmful colours,
availability of safer alternatives at affordable prices with control on the
production and selling of hazardous chemicals by the government will help in
prevention of cutaneous and ocular diseases resulting from the celebration
of this colurful festival References
1.
Dada T, Sharma N, Kumar A. Chemical injury due to colors used at the
festival of Holi. Natl Med J India1997;10: 256.
2.
Velpandian T, Saha K, Ravi AK, Kumari SS, Biswas NR, Ghose S. Ocular hazards
of the colors used during the festival-of-colors (Holi) in India--malachite
green toxicity. J Hazard Mater 2007 Jan 10; 139(2): 204- 8.
3. Ghosh SK, Bandyopadhyay D, Chatterjee G, Saha D. The 'holi' dermatoses:
annual spate of skin diseases following the spring festival in India. Indian
J Dermatol 2009 Jul; 54(3): 240- 2.© 2015
Egyptian Dermatology Online Journal |