|
|
Abstract
Perforating pilomatricoma is a rare variant of
pilomatricoma and clinical presentation is varied. We report 67-year-old
patient with an unusual case of perforating pilomatricoma with clinical
diagnosis of keratoacanthoma.
Introduction
Pilomatricoma is a benign cutaneous neoplasm with
differentiation toward the hair matrix. The tumor presents as a firm
subcutaneous nodule, commonly located on the face, neck, and upper
extremities [1].
Three variants of pilomatricoma have been described morphologically well
defined, anetodermic, proliferating, and perforating. These variants may be
a problem in the clinical differential diagnosis with benign tumours (keratoacanthoma,
foreign body granuloma, pyogenic granuloma) and malignant tumours (squamous
cell carcinoma, dermatofibrosarcoma protuberans, amelanotic malignant
melanoma and cutaneous lymphoma) [2].
We report clinical and morphological features of one
rare case of perforating pilomatricoma arising keratoacanthoma.
Case Report
A 67-year-old man was
referred to our centre with a 2-month history of an asymptomatic nodule on
the left arm. There was no history of trauma. Clinical examination revealed
a central crateriform ulceration lesion or keratin plug that may project
like a horn of 1.5x1.2 cm (fig. 1).
The clinical diagnosis was keratoacanthoma. The histopathological study
showed fully developed lesions show lipping (buttressing) of the edges of
the lesion which overlap the central keratin-filled crater, giving it a
symmetric appearance. In the central area of the lesion presented basaloid
cells with eosinophilic cytoplasm and eosinophilic shadow cells (fig
2 and 3). Calcification sites were also noted.
The diagnosis perforating pilomatricoma was made and was excised. No
recurrence was noted 1 year later.
 | Fig 1:
Erythematous lesion show an elevated border with a central
ulceration covered with crusts. |
|
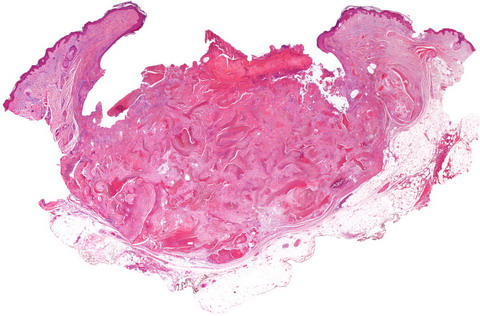
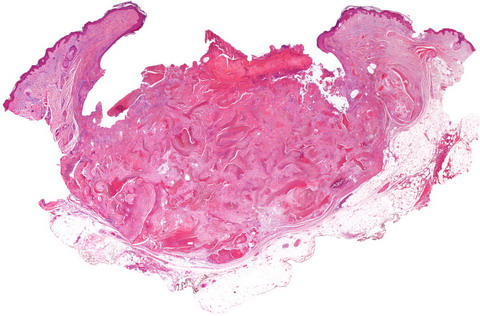 | Fig
2: The epidermis adjacent to tumor is invaginated, forming kind
of buttress, and connected to pilomatricoma (H&E Panoramic). |
|
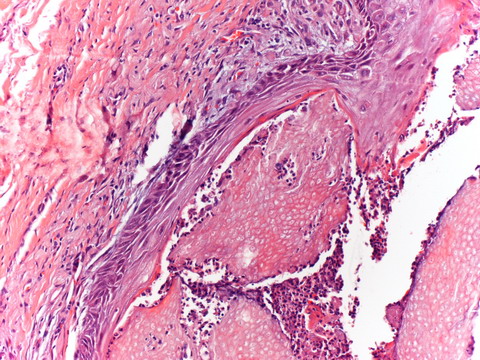
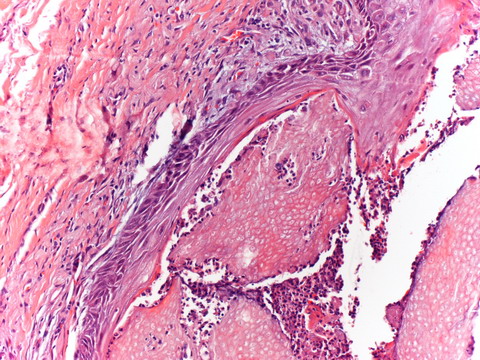 | Fig
3: Present islands of eosinophilic shadow cells perforating to
epidermis (original magnification, H&E x200). |
|
Discussion
The first complete work, based on a series of patients
was published by Malherbe 1880, described calcifying epitheliomas. The
pilomatricoma is a common benign cutaneous adnexal tumor and is
histologically composed of 3 types of cells: basophilic cells with deeply
basophilic nuclei and scanty cytoplasm; shadow cells with a central
unstained area; and transitional cells between the former 2 types of cells.
There are several clinical types of pilomatricoma:
perforating, bullous, melanocytic, giant, keratoacanthoma-like, exophytic,
anetodermic, lymphangiectatic, multinodular, malignant, symmetrical
involvement and multiple [2].
Three variants of pilomatricoma have been described
morphologically well defined: anetodermic [3],
proliferating [4],
and perforating [5].
The variant perforatoring pilomatricoma is a lesion is
extremely rare, had been only reported 14 cases in the English literature.
In our case the lesion in the panoramic has a crater with raised edges
pattern, justifying the clinical diagnosis of keratoacantoma.
The phenomenon "perforating" has been termed
transepithelial elimination. The mechanism of epidermal perforation said
that the superficial location may be one of the causative factors in
transepidermal elimination [6].
The pathological tissue behaves as a mechanical irritant and causes
hyperplasia of the epidermis and epithelium of the hair follicle. Epithelial
hyperplasia encloses the pathological tissue, which is gradually brought
towards the surface and is finally eliminated with the keratinocytes [7].
There are types of lesions with transepidermal
elimination as osteoma cutis which is a rare lesion characterized by the
presence of the bone tissue within the dermis and/or hypodermis [8];
perforating granuloma annulare which is characterized by the transepidermal
elimination of degenerated (necrobiotic) collagen fibers [9];
elastosis perforans serpiginosa which is a rare skin disease in which
abnormal elastic tissue fibers, other connective tissue elements, and
cellular debris are expelled from the papillary dermis through the epidermis
(transepithelial elimination) [10];
perforating folliculitis which is a topical skin condition that resembles
regular folliculitis but instead has a keratin, or harder skin, core [11].
In our case the lesion appeared in a short time,
crater-like apparently giving the clinical diagnosis of keratoacanthoma.
References
1. Julian CG, Bowers PW. A clinical review of 209 pilomatricomas. J Am Acad
Dermatol. 1998; 39: 191- 195.
2. Ciralik H, Coban YK,
Arican O. A case of perforating pilomatricoma. J Dermatol. 2006; 33: 394-
398.
3. Fender AB, Reale VF, Scott GA. Anetodermic
pilomatricoma with perforation. J Am Acad Dermatol. 2008; 58: 535- 536.
4. Niiyama S, Amoh Y, Saito N, Takasu H, Katsuoka K. Proliferating
pilomatricoma. Eur J Dermatol. 2009; 19: 188- 189.
5.
Uchiyama N, Shindo Y, Saida T. Perforating pilomatricoma. J Cutan Pathol.
1986; 13: 312- 318.
6. Kang HY, Kang WH. Guess what!
Perforating pilomatricoma resembling keratoacanthoma. Eur J Dermatol. 2000;
10: 63- 64.
7. Fetil E, Ozkan S, Ilknur T, Erdem Y,
Lebe B, Güneş AT. Multiple pilomatricoma with perforation. Int J Dermatol.
2002; 41: 892- 893.
8. Haro R, Revelles JM, Angulo J,
Fariña Mdel C, Martín L, Requena L. Plaque-like osteoma cutis with
transepidermal elimination. J Cutan Pathol. 2009; 36: 591- 593.
9. De Aloe G, Risulo M, Sbano P, Pianigiani E, Fimiani M. Congenital
subcutaneous granuloma annulare. Pediatr Dermatol. 2005; 22: 234- 236.
10. Wu JJ, Wagner AM. A case of elastosis perforans serpiginosa. Cutis.
2002; 69: 423- 425.
11. Saray Y, Seçkin D, Bilezikçi
B. Acquired perforating dermatosis: clinic-pathological features in
twenty-two cases. J Eur Acad Dermatol Venereol. 2006; 20: 679- 688.
© 2010 Egyptian Dermatology Online Journal |