|
|
Abstract
In the following case report we describe a 66 year-old man who was presented
with a squamous cell carcinoma (epithelial tumour) on the skull which grew
on the scar of a previously surgically excised sarcoma (mesenchymal tumour).
This is the first description of such a coincidence, which may be due to
the development of a mutated stem cell colony, which differentiated in tumour
cells of several lineages.
Case report
The 66 year-old patient presented to our Departments with a 3-month history
of a 0.5 x 1 cm large, erythematous, ulcerated skin lesion over the medial
side of a surgical scar on the left parietal side of the scalp (as shown
in figure 1a). The scar (as shown in figure 1b) was due to surgical
excision of a sarcoma (G2) 5 years ago [1].
At that time the dermatological examination of the patient had detected
a painless solitary 3 x 5 cm large, erythematous swelling (as shown in
figure 2a) and the histopathological examination (as shown in figure
2b) had detected pleomorphic mesenchymal cellular regeneration in the
subcutaneous tissue with a limited nodular process. A focal fibrotic false
capsule had been seen. The tissue had shown myxoid infiltration. An immune
histochemical staining had revealed negative results for CD34, S100, actin,
desmin and pancytokeratin staining, while labeling with the Ki67 antigen
had detected a proliferation rate of 80%. The skull computer tomography
prior to surgical excision of the tumour has shown a localized space-occupying
lesion in the soft tissue without intracranial metastasis. The chest computer
tomography did not reveal any pathological signs.
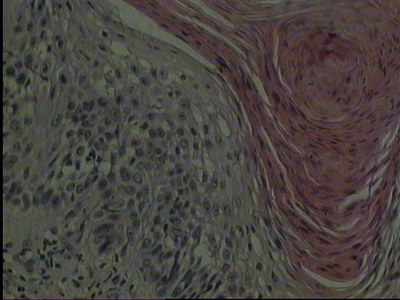
 | Fig 1a:
A 0.5 x 1 cm large, erythematous, ulcerated skin lesion over the
medial side of a surgical scar on the left parietal side of the
scalp before surgical excision. |
|
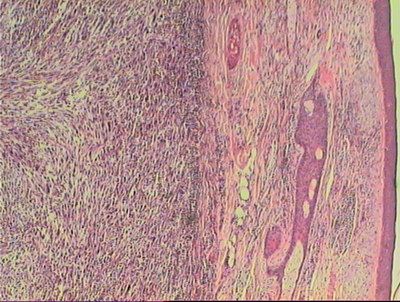
 | Fig 1b:
Histology: Squamous cell carcinoma with a total depth of 0.7 mm.
Orthohyperkeratosis, epidermal hyperplasia with disturbance in
the cell arrangement of the lower epidermal layers associated
with cellular and nuclear polymorphism. Proliferation of
atypical epithelial growth in the upper dermis was seen (hematoxylin
and eosin). |
|
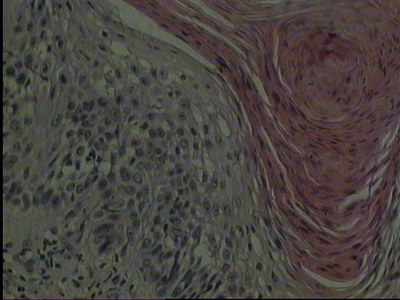
 | Fig
2a: A painless solitary 3 x 5 cm large, erythematous tumour
with teleagiectasia over the left parietal side of the scalp. B)
Sarcoma: pleomorphic mesenchymal cellular regeneration in the
subcutaneous tissue with a limited nodular process (hematoxylin
and eosin). |
|
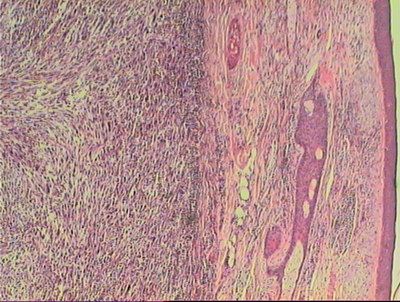 | Fig
2b: A focal fibrotic false capsule can been seen. |
|
 | Fig
2c: The left parietal side of the scalp after surgical
excision. |
|
The regular oncological follow-up of the patient every 6 months has detected
two basal cell carcinomas over the left side of the back and the right lower
limb after 2 years, which were treated surgically with elliptical excisions.
The current lesion on the skull was also detected at the regular follow-up
and was surgically excised. The histological examination showed orthohyperkeratosis,
epidermal hyperplasia with disturbance in the cell arrangement of the lower
epidermal layers associated with cellular and nuclear polymorphism. In addition,
proliferation of atypical epithelial growth in the upper dermis was seen
(as shown in figure 1a). The diagnosis of squamous cell carcinoma
was concluded with a total depth of 0.7 mm. There was no evidence of sarcoma
recurrence. The regional lymph nodes and the chest were free of lesions
in imaging examinations.
Discussion
Soft tissue sarcomas account for 1% of all malignancies. Approximately
60% of soft-tissue sarcomas arise in the extremities. The lower extremities
are three times more often involved than the upper extremities. Further
sites involved are the trunk (19%), the retroperitoneum (15%), and the head
and neck (9%) [2]. Approximately 80% of
head and neck sarcomas occur in adults, whereas the most common subtypes
are osteosarcoma, angiosarcoma, malignant fibrous histiocytoma, and fibrosarcoma,
and 10-20% occur in children, the most common subtype being rhabdomyosarcoma
[3].
On the other hand, squamous cell carcinoma is the second most common
malignancy of the skin after basal cell carcinoma and the skin is the most
common site for squamous cell carcinoma [4].
It accounts for 20% of cutaneous malignancies and 80-90% of all head and
neck cancers [5]. Sun exposure is a major
risk factor for epithelial tumours, while sarcoma growth does not seem to
be related to sun exposure.
In our patient, skin tumours of different lineage, namely squamous cell
carcinoma of epithelial (ectodermal) and sarcoma of mesenchymal (endodermal)
origin, occurred at the same skin region in a period of 5 years the former
developed over the scar of the latter: Such a coincidence has not been reported
before. Since these lesions were the only tumors detected in this patient,
a mutated stem cell colony, which is able to differentiate in cells of several
lineages, could be speculated [6].
References
1. WHO classification of soft tissue tumours. 2006; 10-17.
2. Potter BO and Sturgis EM. Sarcoma of head and neck. Surg
Oncol Clin N Am 12:379-417, 2003.
3. Sidappa KT and Krishnamurthy A. Adult soft-tissue sarcomas
of the head and neck. Indian J Dermatol 48:284-288, 2011.
4. Papadopoulos O, Frantzoglou M, Chrisostomidis C, Konofaos
P, Frangoulis M and Barlas G. Neglected squamous cell carcinoma of the frontal
area: a clinical report. J Craniofac Surgery 17:1015-1020, 2006.
5. Hiu CS, Lin CY, Kuo TT, Kuan YZ, Chen MJ, Ho HC, Yang
LC, Chen CH, Shih IH, Hong HS and Chuang YH. Malignant cutaneous tumors
of the scalp: a study of demographic characteristics and histologic distributions
of 398 Taiwanese patients. J Am Acad Dermatol 56:448-452, 2007.
6. Zouboulis CC, Adjaye J, Akamatsu H, Moe-Behrens G and
Niemann K. Human skin stem cells and the ageing process. Exp Gerontol 43:986-997,
2008.© 2012 Egyptian Dermatology Online
Journal
|