|
|
Abstract
Trichoblastoma is a rare benign adnexal tumour. Cribriform
trichoblastomas are also called trichoepitheliomas which can be of
solitary non-familial type or multiple familial trichoepitheliomas
(MFT). Familial type is also known as Brook -Fordyce disease and is an
autosomal dominant disease. Here we describe a case who presented with
multiple skin colored facial papules and nodules with a history of
similar lesions in other family members. Histopathology confirmed the
diagnosis of trichoepitheliomas. MFT has been linked to genetic
mutations in CYLD gene on chromosome16q12-13 and chromosome 9p.
Introduction:
Trichoblastoma is a benign adnexal neoplasm that differentiates
toward the trichoblast, i.e., the folliculo- sebaceous- apocrine germ,
or follicular germ.[1] There are five
types of trichoblastomas i.e. nodular, retiform, cribriform, racemiform,
and columnar.[2] Cribriform
trichoblastoma is the most common pattern and is another name for
trichoepithelioma.[3] Trichoepitheliomas
present as solitary non- familial lesion or multiple lesions as a part
of autosomal dominant inherited syndrome known as Multiple Familial
Trichoepitheliomas (MFT) or Brook -Fordyce disease.[2]
Brooke and Fordyce first described inherited multiple trichoepitheliomas
in 1892 under the names 'multiple benign cystic epitheliom' and
epithelioma adenoids cysticum' respectively.[3]
Inherited multiple trichoepitheliomas are also present in Brooke-
Spiegler syndrome (BSS) which is also an autosomal dominant inherited
syndrome characterized by cylindromas, trichoepitheliomas, and
occasional spiradenomas. In a family with Brooke- Spiegler syndrome,
some individuals may present with isolated cylindromas or
trichoepitheliomas or both may be present in an individual.[4]
Herein we report a case of multiple familial trichoepitheliomas.
Case report:
A fifteen year old boy presented with multiple skin colored
papulo-nodular lesions located mainly on the central part of the face
around nose (Fig1). Lesions started at the age of ten years and
continued to appear till date. No other cutaneous lesions were present
on other parts of the body. Systemic examination was within normal
limits. Skin biopsy was consistent with the clinical diagnosis of
trichoepithelioma showing lobules of small, dark basaloid cells, with
peripheral palisading surrounding a central area of eosinophilic
amorphous material (Fig 2). There was a history of similar
lesions in the mother, maternal grandmother and great maternal uncle.
The lesions in mother appeared at the age of about sixteen years around
her nose and the whole face was involved within two years (Fig 3).
There was no other significant history in the mother.
 | Fig 1:
Showing multiple centrofacial papulo-nodular lesions in the
index case. |
|
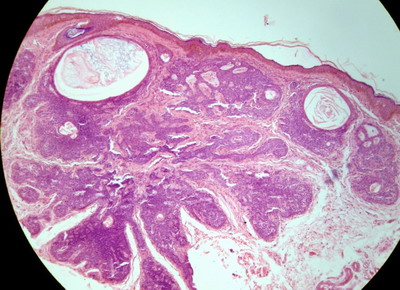
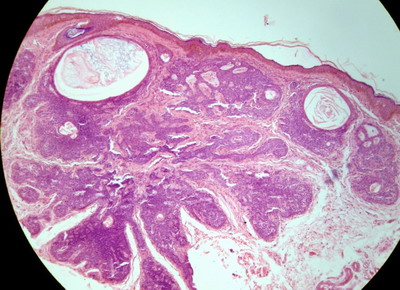 | Fig
2: Histopathology showing lobules of small, dark basaloid
cells, with peripheral palisading surrounding a central area of
eosinophilic amorphous material (H&E X 40). |
|
 | Fig
3: Showing multiple trichoepitheliomas over face in the
mother. |
|
Discussion:
Multiple familial trichoepitheliomas (MFT) usually present between 10
and 20 years of age with multiple skin colored centrofacial papules. [5]
They can increase in number and size, producing significant cosmetic
disfigurement. Although it is an autosomal dominant inherited disease,
it is more common in females due to lessened expressivity and
penetration in males. [6]
There is a genetic heterogeneity of MFT. Initial reports linked MFT
to chromosomes 9p21 but recent reports have found mutation in
cylindromatosis tumor suppressor gene (CYLD), which maps to chromosome
16q12-q13 in most of cases. Mutation in CYLD gene give rise to MFT
indistinguishable from phenotype assigned to 9p21. As Brooke-Spiegler
syndrome is also linked to the CYLD gene so MFT is likely to be a
phenotypic variant of BSS.7Sporadic forms have been linked to gene at
chromosome 9q22.3. [1] In our case
similar type of lesions were present in all family members thus it fits
well in Brook Fordyce's disease.
Multiple trichoepitheliomas also form a part of other rare syndromes
like the Rombo syndrome (vermicular atrophoderma, milia, hypotrichosis,
basal cell carcinomas, trichoepitheliomas and peripheral vasodilatation
with cyanosis) and Basex syndrome (follicular atrophoderma,
hypotrichosis, occasional trichoepitheliomas, basal cell carcinomas, and
localized or generalized hypohidrosis). [4]
Histopathology typically shows horn cysts, tumour islands composed of
basophilic cells of basaloid appearance arranged in peripheral
palisading pattern. [8]
Malignant transformation of these lesions to basal cell carcinoma is
very rare. Any suspicion of malignant change which is indicated by rapid
growth and ulceration in the pre- existing lesions calls for adequate
excision and histological examination. [3]
Treatment is mainly for cosmetic concern. Various treatment
modalities which have been tried include surgical excision, chemical
cauterization, laser resurfacing, electro-surgery and dermabrasion.
Recently, topical 5% imiquimod cream has been advocated as a useful
treatment. [9] CYLD encodes a
deubiquitinating enzyme that negatively regulates the nuclear factor
(NF)-κB
by specific tumour necrosis factors (TNFRs). The NF-κB
transcription factor plays key role in inflammation, immune response,
oncogenesis and protection against apoptosis. Thus inhibition of CYLD
increases resistance to apoptosis, which is responsible for
tumourogenesis. The same mechanism has been supposed to work while
treating MFT, s with adalimumab (a neutralizing antibody to TNF) and
aspirin (inhibitor of NF-
κB). [10] Thus providing medical
therapeutic options in addition to surgical options.
Conclusion:
To conclude, MFT is a relatively uncommon disease. For patients
presenting with multiple centrofacial papules especially with positive
family history, a high index of suspicion is needed to make correct
diagnosis.
References
1. Hurt MA, Kaddu S, Kutzner H, Cribier B, Schulz T,
Hartschuh W. Benign tumours with follicular differentiation. In: LeBoit
PE, Burg G, Weedon D, Alain Sarasin, editors. World Health Organization
Classification of Tumours. Pathology and Genetics of Skin Tumours. Lyon:
IARC Press; 2006. p. 152-3.
2. Khandpur S, Ramam M. Skin Tumors. In: Valia RG, Valia
AR, editors. IADVL Textbook of Dermatology. 3rd ed. Mumbai: Bhalani
Publishing House; 2008. p.1504.
3. Pincus LB, McCalmont TH, Neuhaus IM, Kasper R, Oh DH.
Basal cell carcinomas arising within multiple trichoepitheliomas. J
Cutan Pathol 2008; 35: 59- 64.
4. Szepietowski JC, Wasik F, Szybejko-Machaj G, Bieniek
A, Schwartz RA. Brooke-Spiegler syndrome. J Eur Acad Dermatol Venereol
2001; 15: 346- 9.
5. Fisher GH, Geronemus RG. Treatment of multiple
familial trichoepitheliomas with a combination of aspirin and a
neutralizing antibody to tumor necrosis factor alpha: A case report and
hypothesis of mechanism. Arch Dermatol 2006; 142: 782- 3.
6. Crotty K, Dutta B, Hogan P. Multiple
trichoepitheliomas in a mother and daughter. Australas J Dermatol 2003;
44: 270- 2.
7. Salhi A, Bornholdt D, Oeffner F, Malik S, Heid E,
Happle R, etal . Multiple familial trichoepithelioma caused by mutations
in the cylindromatosis tumor suppressor gene. Cancer Res 2004; 64: 5113-
7.
8. Lee KH, Kim JE, Cho BK, Kim YC, Park CJ. Malignant
transformation of multiple familial trichoepithelioma: case report and
literature review. Acta Derm Venereol 2008; 88: 43-6.
9. Johnson H, Robles M, Kamino H, Walters RF, Lee A,
Sanchez M. Trichoepithelioma. Dermatol Online J 2008; 14(10): 5.
10. Yiltok SJ, Echejoh GO, Mohammad AM, Ituen AM,
Igoche MI, Dades OT. Multiple familial trichoepithelioma: a case report
and review of literature. Niger J Clin Pract 2010; 13: 230- 2.© 2012 Egyptian Dermatology Online
Journal
|