|
|
Abstract
We present a case of a 20-year-old
girl in whom plasma cell panniculitis with morphea-like clinical manifestation
was diagnosed. She had hyperpigmented indurations
over the inner aspects of both thighs extending to the pubic area, causing
mild labial swelling, down to the inner aspects of both knees. Skin biopsy
showed plasma cell panniculitis favoring a diagnosis of morphea profundus.
Another sibling had generalized subcutaneous nodules (2-4 cm, non-tender,
mobile, particularly in the head and trunk) with alopecia overlying the
scalp lesions. and skin biopsy showed lupus panniculitis. Family history
of consanguinity was present, but both parents were unaffected. To our knowledge
this is the second report of autosomal recessive plasma cell panniculitis
with the clinical manifestations of morphea.
Introduction
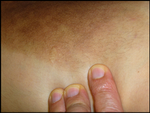
A 20-year-old female
(patient a) had a 5-year history of slowly progressive, several brown
asymptomatic plaques
over the inner aspects of both thighs extending to the pubic area and
down to the inner aspects
of both knees. Her general health was good and her physical
examination revealed
well demarcated, nontender, hyperpigmented induration over the inner
aspects of both thighs
extending to the pubic area, causing mild labial swelling, and extending
caudally to the inner aspects of both knees (Fig 1, 2, 3). Mild hypertrichosis
was observed over the thigh plaques. Musculoskeletal and neurologic examinations
were normal.
|
|
|
|
| Fig 1,2,3:
Patient (a) showing hyperpigmented induration over the inner
aspects of both thighs extending to pubic area, causing
mild labial swelling, and down to the inner aspects of both
knees. Mild hypertrichosis
was observed over the thigh plaques |
|
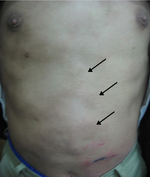
Her 18-year-old brother
(patient b) had a 6-month history of generalized subcutaneous nodules and
a history of a previous attack of the same lesions one year ago. His general
health was not impaired and his physical examination revealed generalized
subcutaneous nodules (2-4 cm, nontender, mobile, particularly in head and
trunk) with alopecia overlying the scalp lesions (Fig 4,5,6). In
musculoskeletal examination he had also generalized arthralgia with the
difficulty of movement while the neurologic examination was normal. A history
of consanguinity was present; the parents were first-degree cousins. Laboratory
workup of both siblings included complete blood count and differentiated
blood count, ESR, C reactive protein (CRP), blood urea nitrogen, creatinine,
liver function tests, lipid profile, ANA, ds DNA, Rheumatoid Factor (RF),
Serum Protein Electrophoresis and Borrelia antibody titer. Laboratory data
were noncontributory except for an elevated ESR [patient (a): 45 mm/h; patient
(b): 75 mm/h], CRP [patient (a): +; patient (b): ++], ANA [patient (a):
1:80 speckled pattern; patient (b): 1:160 speckled pattern], RF [patient
(a): -; patient (b): +], Hyper gammaglobulinemia
was Positive for both of siblings and ds DNA was Negative for them.
|
|
|
|
| Fig 4,5,6:
Patient (b) showing generalized subcutaneous nodules (2-4
cm, mobile, particularly in head and trunk) that seen alopecia
on the lesions of scalp. |
|
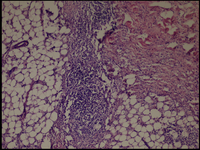
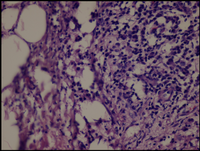
The histologic sections
of [patient (a), taken by punch biopsy (4mm) from right thigh] revealed
superficial and deep, intense plasma cellular and lymphocytic infiltrate,
primarily in the lower dermis and fat septae with spillover to the fat lobules.
Fibrosis was present in the deep dermis and in the fat. There was no vasculitis.
(Fig 7,8).
|
|
|
| Fig 7,8 :
The histologic sections of [patient (a), taken by punch
biopsy (4mm) from right thigh] revealed superficial and deep,
intense plasma cellular and lymphocytic infiltrate, primarily
in the lower dermis and fat septae with spillover to the
fat lobules. Fibrosis was present in the deep dermis and
in the fat. There was no vasculitis. (H&E stain; original
magnifications: x 40) |
|
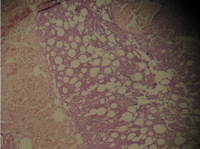
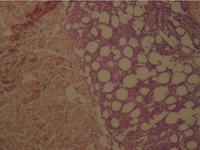
The histologic sections
of [patient (b), taken by punch biopsy (4mm) from trunk] revealed superficial
and deep perivascular lymphocytic infiltrate with plasma cells in the dermis.
Deep lymphocytic infiltration in the fat lobules and in the septa and
hyaline necrosis of the fat was present. There was no vasculitis. (Fig
9,10).
|
|
|
| Fig 9,10:
The histologic sections of [patient (b), taken by punch
biopsy (4mm) from trunk] revealed superficial and deep perivascular
lymphocytic infiltrate with plasma cells in the dermis.
Deep lymphocytic infiltration in the fat lobules and in
the septa and hyaline necrosis of the fat was present.
There was no vasculitis. (H&E stain; original magnifications:
x 40) |
|
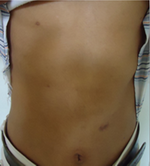
Patient (b) was treated
with prednisolone 25 mg/d for 3 month and then tapered, which reduced number
of sub cutaneous nodules. Skin biopsy was repeated and it showed L.E Panniculitis
with significant reduction in the intensity of infiltration. His ANA titer
dropped from 1:160 to 1:40. He was visited a year after treatment
(Fig 10,11,12); no disease progression
was seen. He was lost to follow-up.
|
|
|
|
| Fig 11,12,13:
Patient
(b) was treated with prednisolone 25 mg/d for 3 month and
then tapered, which reduced number of sub cutaneous nodules.
Skin biopsy was repeated and it showed L.E Panniculitis
with significant reduction in the intensity of infiltration.
He was visited a year after treatment; no disease progression
was seen. He was lost to follow-up. These pictures was taken
2 month after treatment |
|
Patient (a) was
treated with prednisolone 25 mg/d for 7 month and then tapered, which reduced
induration of
the skin, and swelling of the labia. No further improvement was noticed
after 6 months of treatment. Methotrexate 7.5 mg/wk was added, which helped
in further reduction of induration. When she failed to show further improvement
methotrexate was discontinued after 5 month. Skin biopsy was repeated, and
it showed Plasma cell Panniculitis with no significant change in the
intensity of infiltration. This persistent extensive plasma cell infiltrate
for 5 years in the absence of clinical disease progression is intriguing
because the inflammatory infiltrate is observed at the onset of morphea and
with time, inflammation is replaced by fibrosis. Her ANA titer dropped from
1:80 to 1:40. She was visited a year after treatment; her skin lesions remained
unchanged with no further disease progression.
Discussion
The term morphea
profunda was suggested by Person and Su [1]. They described
a group of (23) patients with generalized morphea in whom a dense inflammatory
cell infiltrate in the subcutis and underlying fascia was associated with
extensive sclerosis and hyalinization of the connective tissue at this level.
The infiltrate consisted of both lymphocytes and plasma cells. In morphea
profunda, there is marked thickening of fibrous tissue in the deeper dermis,
with moderate to marked inflammatory infiltrate consisting primarily of
lymphocytes and
occasional eosinophils
around small vessels in the dermis and in the Panniculus. This disorder
differs from Morphea in that Morphea Profunda has deeper involvement and
a more pronounced inflammatory infiltrate. Plasma cells usually are less
numerous; however, plasma cells as a predominant cell type in Morphea Profunda
have been reported earlier [2]. In patient (a), Morphea
Profunda appeared to be the most likely diagnosis because of the extensive
subcutaneous thickening and hyperpigmentation without systemic involvement.
However, the presence of identical clinical features and a histologic picture
of plasma cell panniculitis was puzzling. A family history of consanguinity,
unaffected parents, and disease manifestation in two
siblings
strongly suggest an autosomal recessive inheritance. The clinical picture
of our patient is similar to a case
reported by Issam R. Hamadah et al,[3] and Koji Sayama
et al, [4] but in contrast to the former there was no lateral
scalloping deformity of the buttocks in our patient. Vincent et al, [5]
reported plasma cell panniculitis in a patient with Linear Scleroderma.
The presence of plasma cells suggests a role of humoral immunity in the
pathogenesis of Morphea and Scleroderma.
References
1. Person JR, Su WPD. Subcutaneous morphea: a clinical study
of sixteen cases. Br J Dermatol 1979;100:371-80.
2. Whittaker SJ, Smith NP, Russell Jones R. Solitary morphea
profunda. Br J Dermatol 1989;120:431-40.
3. Issam R. Hamadah et al, Autosomal recessive plasma cell
panniculitis with morphea-like clinical manifestation. J Am Acad Dermatol
2006;54:S189-91.
4. Sayama K, Chen M, Shiraishi S, Miki Y. Morphea profunda.Int
J Dermatol 1991;30:873-5.
5. Vincent F, Prokopertz R, Miller RAW. Plasma cell paniculitis:
a unique clinical and pathological presentation of linear scleroderma. J
Am Acad Dermatol 1989;21:357-60.© 2014
Egyptian Dermatology Online Journal
|