|
|
Abstract
Background: Verrucous epidermal nevi (VEN) are benign congenital
epidermal hyperplasia and they constitute the most frequent form of
epidermal nevi. Verrucous epidermal nevi lesions typically occur on the
trunk or extremities but may also occur on the face and neck. The lesions
may vary from skin colored to brown. No ideal treatment is yet available.
Objective: To evaluate the efficacy and safety of long pulsed Nd:
YAG laser (1064 nm) in treatment of verrucous epidermal nevus. Patients
and methods: This study was conducted on twenty-one patients with
verrucous epidermal nevi. They were subjected to treatment with long pulsed
Nd: YAG laser (1064 nm) with 5mm spot size, 110J-150J/cm² fluence and
20-40msec pulse duration. A part of each lesion was subjected to laser
treatment and the other part was left untreated as a control. Sessions were
performed monthly for a maximum of 6 months. Evaluation included clinical,
histological, and patient self assessment. Follow up was carried for 6
months after the last session. Results: Patients received a mean
of 4.48 ±1.33 sessions. Eight patients (38.1%) showed an excellent
improvement, 9 patients (42.9%) had good improvement, and 4 patients (19%)
had moderate improvement. Hypopigmentation was reported in one patient with
skin type V. No recurrence was reported during the follow up period. After
treatment with Nd: YAG laser, the histopathology revealed orthokeratosis, a
thinned epidermis, sparse superficial perivascular lymphohistiocytic
infiltrate and a normal capillaries appearance. Before treatment the mean
±SD of epidermal thickness was 169.5±22.9µm (range 209-138 µm) which reduced
significantly to 69.8±15.5 after treatment (P<0.001). Conclusion:
Long pulsed Nd: YAG laser is successful modality for treatment of verrucous
epidermal nevus with no scarring and less downtime healing. However, further
studies are necessary to refine the procedure and to confirm the present
encouraging findings; also longer periods of follow up are needed.
Introduction
Epidermal nevi are hamartomas of the skin and have multiple clinical
variants, including a verrucous type [1].
Verrucous epidermal nevi (VEN), constitute the most frequent, form, however,
three other forms of epidermal nevi can be distinguished; inflammatory
linear verrucous epidermal nevus (ILVEN), Darier- like epidermal nevus and
linear porokeratosis [2]. Verrucous
epidermal nevi occur in circumscribed patches or more often, in linear
streaks or whorls following Blaschko's lines [3].
The lesions typically occur on the trunk or extremities, but may also occur
on the face and neck [1]. Clinically, flat,
velvety, papillomatous nevi developed in the newborn and have been
distinguished as 'soft', whereas, more keratotic, verruciform lesions
occurred during adolescence and were described as 'hard' [1,2].
The lesions may vary from skin- colored to brown [2].
Histologically, keratinocytic, or verrucous epidermal nevi are characterized
by acanthosis, orthohyperkeratosis, papillomatosis, and an expanded
papillary dermis which is sharply demarcated from the surrounding normal
skin [2]. Analyzing 167 biopsy specimens
from 160 patients with epidermal nevi, excluding nevus sebaceous, verruca-like
features were described in (2%) and dilatation of blood vessels have been
found [4]. Patients usually seek advice
because of the disfiguring cosmetic appearance [2].
No ideal treatment is yet available, the topical treatments such as combined
therapy of retinoic acid and 5-fluorouracil, dithranol, occlusive topical
steroids, chemical peels and podophyllin may improve the keratotic surface
however, they always correlate with high rate of recurrence [5].
On the other hand, more aggressive approaches such as cryosurgery, electro-cautery
and dermabrasion are used but recurrence is common if the damage is
superficial and hypertrophic or hypopigmented scarring can occur if a
significant proportion of reticular dermis is removed [6].
In the last three decades, multiple modalities of laser treatment have been
tried; however, very few studies reported comparative results. Based on
selective photothermolysis, pigment-specific lasers can be used to achieve
significant cosmetic improvement of dark epidermal nevi with a reduced risk
of scarring, but successful treatment was not achieved in non-pigmented or
keratotic lesions [7]. Ablative lasers, such
as CO2 laser and erbium-YAG laser have been used for the treatment of
superficial epidermal pigmented lesions [6,8].
Their wavelengths are absorbed by both intra- and extracellular water of the
epidermis and dermis, which results in a non-specific destruction [8-10].
There is a relatively narrow margin of safety when treating epidermal nevi;
if the treatment is too superficial with removal of the epidermis only, the
nevus will recur and if it goes too deeply into the reticular dermis,
hypertrophic scaring may develop [11]. In
Previous studies, 585-nm Pulsed dye laser (PDL) has been used successfully
in treatment of inflammatory linear verrucous nevus (ILVEN), which is a
variant of epidermal nevi, by destructing the dilated blood vessels and
decreasing the inflammatory process [12,13].
Based on the postulation that oxyhemoglobin in blood vessels has strong
absorption peaks at wavelengths ranging from 585 to 595 nm of PDL and
moreover has a significant, albeit more modest, absorption peak between 800
and 1,100 nm, long pulsed Nd -YAG laser (1064nm) have been used in the
treatment of vascular defects as telangiectasia, portwine stains,
haemangioma, spider nevi, varicose veins [14,15]
and other entities with an associated blood supply including verrucous
lesions such as warts [16]. Therefore, this
study was designed to evaluate the efficacy and safety of long pulsed Nd:
YAG laser in treatment of verrucous epidermal nevus with the target its
blood vessels. Patients and Methods
During the period from September 2008 to August 2009, this study was
conducted on twenty-one patients (9 males, 12 females), with verrucous
epidermal nevi in the Outpatient Clinics, National Institute of Laser
Enhanced Sciences, Cairo University, Egypt. The age of the patients ranged
from 5-20 years. The duration of the disease ranged from 2 -16 years.
Patients were of skin type III, IV, and V. No previous treatment had been
received by any of the patients. Lesions distribution is shown in table 1.
Before starting treatment, an informed written consent was obtained and
photo documentation was carried out. They were subjected to treatment with
long pulsed Nd: YAG laser (1064 nm Cool Glide Excell; Altus Medical
Burlingam, CA) with 5 mm spot size, 110J-150J/cm² fluence and 20-40 msec
pulse duration with contact cooling. The fluence and pulse duration differed
for each patient, depending upon thickness of the lesions, skin type and a
previously performed spot test. Flat, velvety Lesions were treated with
lower fluences and short pulse duration (110J-130J/cm2, 20-30ms), whereas,
hard hyperkeratotic lesions were treated with higher fluences and longer
pulse duration (130J-150L/cm2, 30-40ms). Patients with skin type V were
treated with lower parameter settings even when their lesions were hard and
hyperkeratotic. The laser beam was fired through a cooled sapphire window
with a diameter of 10 mm. For each laser pulse, pre-cooling of the lesion
was achieved by contact cooling using the gold plated cooling head of the
laser's hand piece for 3-5 seconds; the window was kept in contact of the
skin surface for 5 seconds. The laser pulse was delivered followed by
cooling for additional 2 seconds. The process was repeated in the same
manner before and after application of each laser pulse to protect the
epidermis. The sapphire window was continuously cooled by a surrounding
gold-platted copper ring containing circulating water at approximately 51◦C.
Overlapping of 2-3 pulses were needed in order to establish the grayish
discoloration of the lesion that marks the end point of the treatment
session. Steel eye shield was used during laser session for one patient
with infra-orbital lesion to protect the eye globe while the rest of the
patients had their eyes protected by the ordinary opaque plastic goggles.
Treatment was carried out under local anesthesia with lidocaine/prilocaine (EMLA)
cream applied in an occlusive dressing approximately 1 hour before the start
of the laser session. For larger lesions, a representative part of the
lesion was treated and similar size was left as a control according to the
size and location of the lesions. Sessions were performed monthly for a
maximum of 6 months. Patients were evaluated at 5 to 10 days after treatment
to identify any adverse events. Patients stopped to receive sessions at any
time during the protocol of treatment when no further improvement was
observed by either doctors or patients for 2 subsequent sessions. After
treatment, a cream (Fusidic acid 2%+Betamethasone 0.1% preserved with
chlorocresol) was prescribed to patients for 2-3 days following each
session. Sunscreen creams were also recommended depending upon the exposure
of the lesion site to sun. Follow up was carried for 6 months after the last
session. Evaluation procedures Clinical assessment:
This included photographic documentation with digital camera; Kodak DX 3700,
3.1 Mega pixels, 3xs zoom was conducted before and after treatment. Patients
were asked to report any adverse effect. The degree of improvement was
determined as the percent of reduction in the clinical signs; which include
reduction in the size, pigmentation and texture relative to the control
(untreated site) in gradation of 10% to 100% rating. Excellent improvement
is considered to be from 90%-100%, good improvement from 50%-89%, moderate
improvement from 20%-49%, and poor from 0-19% [17].
The percentage reduction evaluations were based on the subjective appearance
of the treatment sites, not on actual measurements.
Histopathological assessment: This was done using three mm punch
biopsies, obtained from lesions before and after treatment, stained by
hematoxylin and eosin (H&E). Microscopic Image analysis for
histopathological samples: The data were obtained using Leica Qwin
500 image analyzer computer system (England). The image analyzer consisted
of a colored video camera , colored monitor, hard disc of IBM personal
computer connected to the microscope , and controlled by Leica Qwin 500
software The image analyzer was first calibrated automatically to convert
the measurement units (pixels) produced by the image analyzer program into
actual micrometer units. The epithelial thickness was measured in each
specimen using the interactive measuring menu with an objective lens of
magnification 10 i.e. of total magnification 100. Readings were obtained
from each specimen & the mean values were calculated in pre & post laser
treatment. The data obtained were subjected to statistical analysis using
Student's t- test Patient self assessment: This was
conducted to grade the overall satisfaction with treatment one month after
the last session. The satisfaction scale simply was done asked each patient
about being very satisfied, satisfied, or not satisfied with the degree of
lesion regression by comparing lesions photographs before and after
treatment . Statistical analysis: The data were coded and
tabulated using the statistical package SPSS version 17.0.The data were
described using the percent for qualitative data. "Pearson's product moment
correlation coefficient" test is used to measure the correlation (linear
dependence) between two variables giving a value between +1 and -1
inclusive. Results
Clinical results: Twenty-one patients presented with lesions of
verrucous epidermal nevi of different sizes, thickness and at different
anatomical sites. The mean age of patients was 12.76 ± 4.4 years (range 5-20
years). They were 12 females (57.1%) and 9 males (42.9%). Fitzpatrick skin
type III was in 6 patients (28.6%), IV in 12 patients (57.1%), and V in 3
patients (14.3%). Mean duration of lesions was 7.48 ± 3.9 years (range 5-20
years). The most frequent location was on the trunk in 5 patients (23.8%),
followed by the face in 4 patients (19%), upper limbs (arms) in 3 patients
(14.3%), axilla in one patient (4.8%), lower limbs (2 thighs ,1 leg) in 3
patients (14.3%), genitalia (2 vulva, 1 scrotum) in 3 patients (14.3%), and
buttocks in 2 patients (9.5%).Clinical data of patients and lesions
distribution were shown in table 1. Assessment of clinical
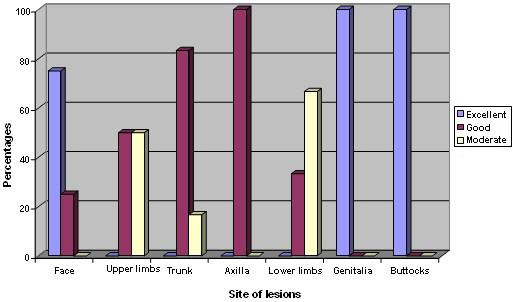
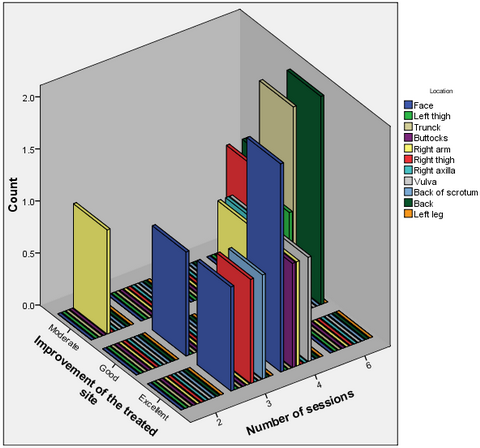
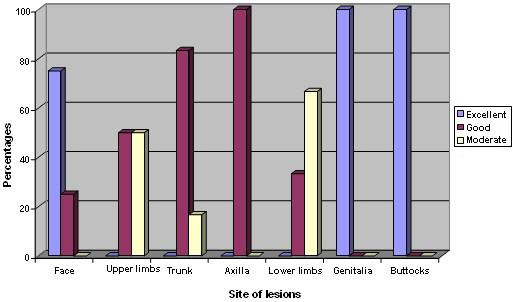
improvement: Site of lesions Out of 21 patients; 8 patients
(38.1%) showed excellent improvement, 9 patients (42.9%) had good
improvement, and 4 patients (19%) had moderate improvement (table 2).
Excellent results were achieved in 8 lesions; 3 (14.3%) lesions on the face,
2 (9.5%) on the buttocks, and 3 (14.3%) on the genitalia (2 vulva, 1
scrotum). Good results were achieved in 9 lesions; 4 lesions (19%) on the
trunk, 2 (9.5%) lesions on the upper limb (arms), and one lesion (4.8%) on
each of the following sites; the face, lower limb (thigh) and axilla.
However, moderate results were obtained in 4 lesions; 2 lesions (9.5%) on
the lower limbs (leg and thigh), and 2 lesions (9.5%) on the trunk and arm
(fig 1). There were no treated sites that showed no improvement or
poor results were obtained in this study. Improvement of the hard elevated
lesions was gradual flattening of the lesions followed by shrinkage of the
lesion. Improvement of soft velvet lesions were elicited by a decrease in
size. Hypopigmentation was reported in one patient (4.8%) with skin type V.
Clinical assessment efficacy was supported by comparing the pre and post
treatment photographic documentation (fig 2-4). In comparison the
untreated control sites showed no improvement. Follow up the patients was
carried on for 6 months after the last laser session without recurrence.
|
Variable |
Patients number |
Percentage |
|
Gender |
female |
12 |
42.90% |
|
|
male |
9 |
57.10% |
|
Skin type |
III |
6 |
28.60% |
|
|
IV |
12 |
57.10% |
|
|
V |
3 |
14.30% |
|
Site of lesions |
Face |
4 |
19% |
|
|
Trunk |
5 |
23.80% |
|
|
Upper limb |
3 |
14.30% |
|
|
axilla |
1 |
4.80% |
|
|
Lower limb |
3 |
14.30% |
|
|
genitalia |
3 |
14.30% |
|
|
buttocks |
2 |
9.50% |
Table1. Clinical data of patients
 | Fig 1:
Percentages of the degree of lesions improvement in regards to
lesions distribution. |
|
|
Site of lesions |
Number of Patients (percentage %) |
|
Excellent |
Good |
Moderate |
Total |
|
Face |
3 (14.9%) |
1 (4.8%) |
- |
4 (19%) |
|
Trunk |
|
4 (19%) |
1 (4.8%) |
5(23.8%) |
|
Upper limbs |
- |
2 (9.5%) |
1 (4.8%) |
3(14.3%) |
|
Axilla |
- |
1 (4.8%) |
|
1 (4.8%) |
|
Lower limbs |
|
1 (4.8%) |
2 (9.5%) |
3(14.3%) |
|
Genitalia(vulva& scrotum) |
3 (14.9%) |
- |
- |
3(14.3%) |
|
Buttocks |
2 (9.5%) |
- |
- |
2 (9.5%) |
|
Total |
8 (38.1%) |
9 (42.9%) |
4 (19%) |
21(100%) |
|
*Average improvement (percentage) |
95% |
70% |
35% |
|
* Excellent improvement
(90%-100%), good improvement (50%-89%), moderate improvement (20%-49%)
Table2: The number of patients (percentage) regarding the site of lesion
and degree of improvement
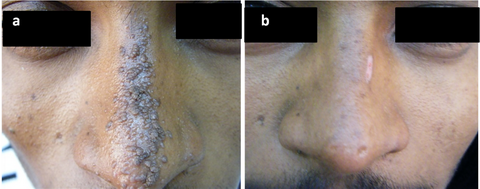
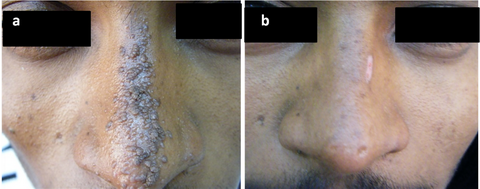 | Fig
2: twenty years- old patient with VEN on the nose (a)
before treatment and (b) excellent improvement after 4 sessions,
hypo-pigmentation appeared in the upper right side. |
|
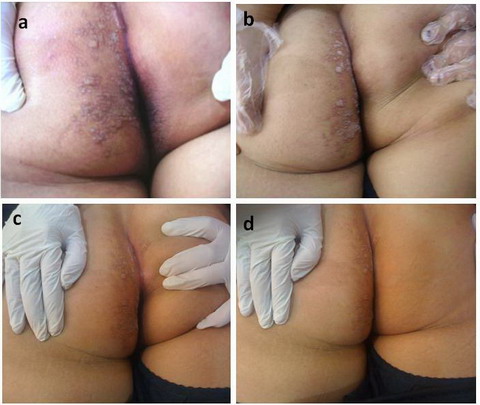
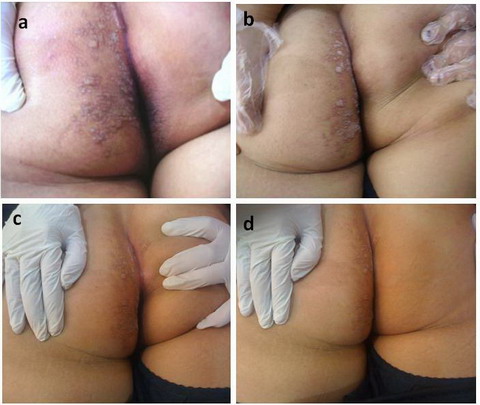 | Fig
3: Twelve
year-old female patient with VEN on the buttocks; (a): before
treatment, (b): after 2 sessions, (c): the left lower inner
medial part is the control site and (d): after treatment. The right
lateral part has received 4 sessions showing excellent result. |
|
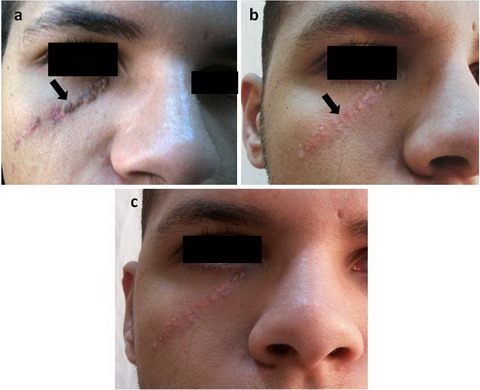
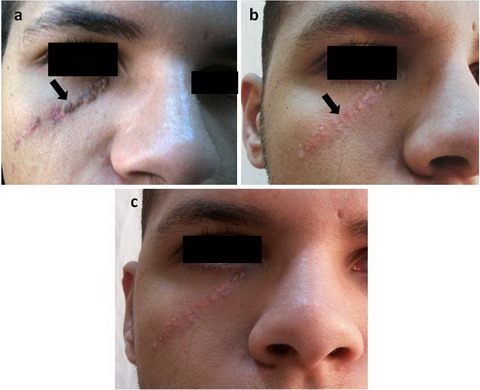 | Fig
4: Nineteen year-old male patient with VEN on the face; (a): the
lower treated part after 2 sessions, (b) showed excellent improvement
of the lower part after 4 sessions and (c) the upper part has been
done for the patient during the follow up period to give him better cosmetic
appearance (the arrow showed demarcation between lower part (treated) and
upper part. The arrow pointed to the site of biopsy. |
|
Number of sessions
Patients received a mean of 4.48 ±1.33 sessions (range 2-6 sessions). Four
patients (19%) received 3 sessions, 9 patients (42.9%) received 4 sessions
and 8 patients (38.1%) received 6 sessions. It has been observed that
excellent improvement was obtained in 3-4 sessions in lesions located on the
face, genitalia and buttocks however this was statistically insignificant.
The relationship between the number of sessions, degree of clinical
improvement and sites of the lesions was shown in fig 5.
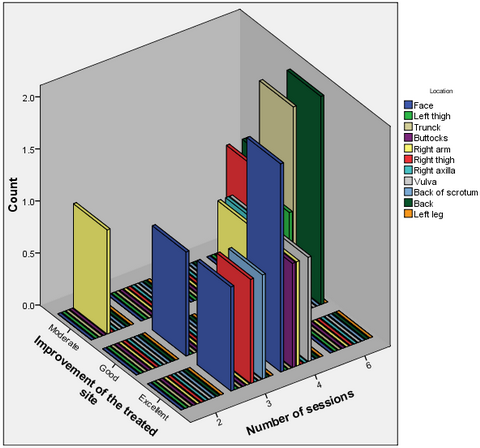 | Fig
5: The relation between improvement of treated sites, number of
sessions. |
|
Correlations between the degree of improvement and site of lesions
"Pearson's product moment correlation coefficient" test was used to measure
the correlation between the degree of improvement and the site of lesions. A
positive correlation was found between the excellent degree of improvement
and the face (r=0.959, p = 0.182), the genitalia (r=0.814, p= 0.394) and the
buttocks (r=0.814, p= 0.394) however this was statistically insignificant
(table 3).
|
Site |
R |
p |
|
Face |
0.959 |
0.182 |
|
upper limbs |
-0.814 |
0.394 |
|
Trunk |
-0.094 |
0.94 |
|
Axilla |
0.096 |
0.939 |
|
Lower limbs |
-0.995 |
0.061 |
|
Genitalia |
0.814 |
0.394 |
|
Buttocks |
0.814 |
0.394 |
Table 3: Correlation between the degree of
improvement and site of lesions done by Pearson's product moment correlation
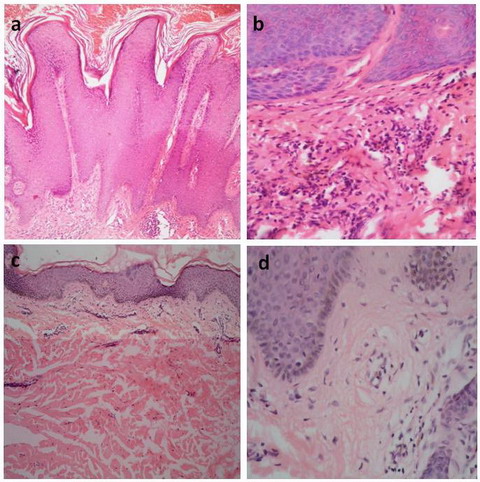
coefficient Histopathological results:
(fig 6) Before treatment, histopathological examination showed
epidermal hyperplasia, papillomatosis, hyperkeratosis, dilated blood vessels
and perivascular lymphohistiocytic infiltrates in the superficial dermis
(fig 6 a, b). After treatment with Nd: YAG laser, the histopathology
revealed orthokeratosis, a thinned epidermis (fig 6 c, d), sparse
superficial perivascular lymphohistiocytic infiltrate and a normal
capillaries appearance. The papillary collagen was highly packed; coarse and
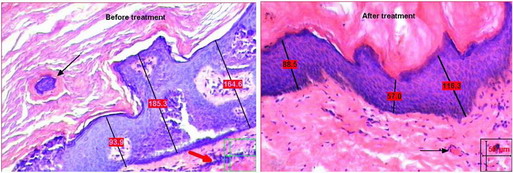
clumped (fig 6 c). Epidermal thickness was measured before
treatment and after Nd:YAG laser treatment as shown in fig 7 a, b .
Before treatment the mean ± SD of epidermal thickness was 169.5 ± 22.9µm
(range 209-138 µm) which reduced significantly to 69.8 ± 15.5 after
treatment (P<0.001) (table 4).
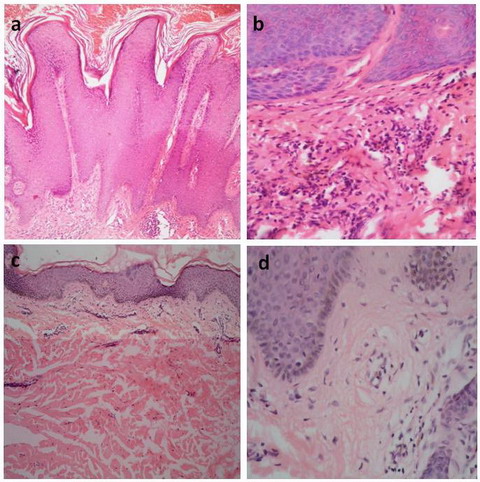 | Fig
6: (a) before
treatment showing epidermal hyperkeratosis, acanthosis and papillomatosis
(H&E x100), (b) before treatment showing mild perivascular
lymphohistiocytic infiltrates in the superficial dermis and dilated
capillaries (H&E x400), (c) after treatment showing orthokeratosis
and thinned epidermis with reduction of papillomatosis (H&E x100), (d)
after treatment showing sparse superficial perivascular lymphohistiocytic
infiltrates and a reduction in number of blood vessels (H&E x400). |
|
|
*Epidermal thickness |
Before treatment |
After treatment |
|
Maximum |
209.03 |
91.1 |
|
Minimum |
138.7 |
41.5 |
|
Mean±SD |
169.5±22.9 |
69.8±15.5 |
|
P value |
<0.001** |
|
* Epidermal thickness was measured in micrometer (µm)
**
Highly significant
Table 4: Epidermal thickness measurements before and after laser
treatment
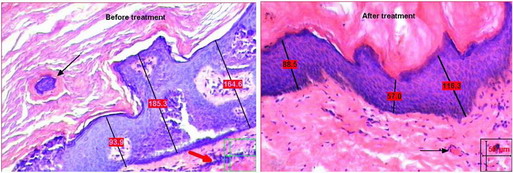 | Fig
7: (a) showed measurements of the
epidermal thickness at different points before treatment. The black arrow
pointed to large thickened blood vessels. The red arrow pointed to the
inflammatory infiltrates. (b) showed reduction in measurements of
epidermal thickness at different points after treatment. The black arrow
pointed to normal blood capillary (H&E x100). |
|
Patients self assessment
results One month after the last laser session each patient graded his
level of satisfaction regarding the improvement of cosmetic appearance using
the photographs taken before and after treatment. Thirteen patients (61.9%)
were very satisfied with the results of treatment, 5 patients (23.8%) were
satisfied and asked for treatment of the whole lesion however and 3 patients
(14.3%) were not satisfied. Discussion
The treatment of verrucous epidermal nevus is difficult and often
un-satisfactory. The multiple treatment modalities that have been used show
that managing this disease is challenging. Ablative lasers such as CO2 and
Erbium-YAG laser have been considered as the gold standard for treatment of
VEN [6,8].
However, vaporization should extend only into papillary dermis; thus, thick,
verrucous lesions may be unresponsive or produce hypertrophic scars, owing
to the unpredictable penetration of the laser beam through the verrucous
tissue [8]. In addition, the expected
outcome after healing is hypopigmentation especially in dark skinned
patients [6,9].
Hohenleutner et al [6] reported that poor
results (partial or full recurrence, hypertrophic or keloidal, cosmetically
unacceptable scar) were found in 5 of 12 patients after the continuous-wave
CO2 laser therapy of verrucous epidermal nevi. Literature relating to the
erbium-YAG laser is mainly concentrated on resurfacing techniques; however,
excellent cosmetic results without apparent scarring in patients with
epidermal nevi located in problematic sites, such as the neck and upper
chest have been documented [9]. These could
be due to biases in the selection of cases with superficial or small lesions
as thick, verrucous lesions may not respond or produce hypertrophic scars,
owing to the unpredictable penetration of the laser beam through the warty
tissue and 25% of patients can show a relapse within 1 year after the
treatment [18]. In contrast, lasers such as
the 585-nm PDL have shown good results in the treatment of ILVEN, which is a
variant of epidermal nevi [12,19].
Sidwell et al [13] explained the success of
pulsed dye laser in treatment of ILVEN by destruction of the dermal
capillaries based on the theory of selective photothermolysis [20]
and the reduction in the number of capillaries and inflammatory mediators
reaching the epidermis supports this idea [19].
Two aspects can explain the mechanism of action of long pulsed Nd: YAG laser
in treatment of VEN. First, ILVEN and VEP share the histopathological
features of dermal involvement with a lymphohistiocytic inflammatory
infiltration and dilated blood capillaries of the upper dermis [4].The
Second explanation; oxyhemoglobin is a chromophore which absorbs both
wavelengths; 585nm pulsed dye laser and to a lesser degree, the 1064nm Nd:
YAG laser; allowing the 1064nm wavelength to penetrate deeper (from 3.7 up
to 6 mm) into tissue than visible light, enabling heat delivery to occur
more deeply into the dilated blood vessels [14].
Thus, selective thermal photocoagulation of dermal blood capillaries of VEN
leads to regression of lesions that was elicited clinically, and confirmed
histologically, where marked reduction in epidermal thickness and number of
blood vessels was observed after end of treatment. Nd: YAG wavelength allows
even deeper penetration into the dermis with relative sparing of the
epidermis and because of the minimal-energy absorption by melanin occurs at
this wavelength, darker skin types can be treated with minimal risk to the
epidermis [14,17].
During the treatments the epidermis was effectively protected by the chilled
cooling head of the laser's hand piece that is a component of this laser
equipment thus, excellent pre-operative, and postoperative skin cooling was
achieved together with a constant perfect view of the operative field. Our
results showed healing with no scarring, no downtime a, and a low risk of
adverse effects, compared to the results of the studies done on the ablative
lasers such as CO2 and erbium-YAG [6,8,11].
Hypo-pigmentation has been shown in one patient and it faded out after 4
months. High fluences (130J-150L/cm2) were used to compensate of for the
possible loss of heat as thick hyperkeratotic epidermis increases the
reflection of laser light [21,22].
Long pulse duration (30-40ms) was chosen to occlude large deep blood vessels
nourishing the thicker hyperkeratotic epidermis [23].
Long pulsed Nd: YAG has been used safely with high fluence and with repeated
overlapping pulses. It has been used for treating acne scars using 120J/cm2
fluence where triple pulses were applied to each acne scar [24].
It was observed clinically that the face, buttocks and genitalia (vulva and
scrotum) were the first sites to show the satisfactory results in the least
number of sessions; however this was statistically insignificant due to
small sample size. The elicited improvement can be explained by the fact
that the skin is more vascular and the epidermis is thinner in these sites
so it responded better [22]. Better results
were obtained with early lesions, so early intervention was advised.
Hohenleutner et al [6] conducted that soft
lesions responded better to CO2 laser than hard lesions; however, long
pulsed Nd: YAG laser enabled effective treatment of both soft and hard
lesions by selecting the proper fluence and pulse duration suitable for each
type. Conclusion
Long pulsed Nd: YAG is a successful modality for treatment of verrucous
epidermal nevus with no scarring and minimal downtime. However, further
studies are necessary to refine the procedure and to confirm the present
encouraging findings, longer periods of follow up, are needed.
Acknowledgment
The authors would like to thank Dr. Fatma Abd Alsalam and Dr. Maha
Sultan; lecturers in dermatology department, Azhar University for their help
in the pathology work. References
1.
Vujevich JJ, Mancini AJ. The epidermal nevus syndromes: Multisystem
disorders. J Am Acad Dermatol. 2004; 50: 957- 961.
2.
Pierson D, Bandel C, Ehrig T et al. Benign epidermal tumors and
proliferations. In: Bolognia JL, Jorizzo JL, Rapini RP, eds. Dermatology.
Philadelphia: Mosby, 2003: 1697- 1720.
3. Bolognia
JK. Lines of Blaschko's. J Am Acad Dermatol 1994; 31: 157.
4. Su WP: Histopathologic varieties of epidermal nevus. A study of 160
cases. Am J Dermatopathol 1982; 4: 161- 170
5. Fox
BJ, Lapins NA. Comparison of treatment modalities for epidermal nevus: a
case report and review. J Dermatol Surg Oncol 1983; 9: 879- 885.
6. Hohenleutner U, Wlotzke U, Konz B, Landthaler M. Carbon dioxide laser
therapy of a widespread epidermal nevus. Lasers Surg Med 1995; 16: 288- 291.
7. Baba T, Narumi H, Hanada K, Hashimoto I. Successful treatment of
dark-colored epidermal nevus with ruby laser. J Dermatol 1995; 22: 567- 570.
8. Park JH, Hwang ES, Kim SN, kye YC. Er-YAG laser treatment of verrucous
epidermal nevus. Dermato Surg 2004; 30 (3): 378- 381.
9. Thual Ni, chevalier JM, Vuillamie M, Tack B, leroy D, Dompmartin A. CO2
laser therapy of verrucous epidermal nevus. Ann dermatol venereol 2006; 133
(2): 131- 138.
10. Boyce S. CO2 laser treatment of
epidermal nevi: Long- term success Derm Surg 2002; 28: 611.
11. Alam M, Arndt KA. A method for pulsed carbon dioxide laser treatment of
epidermal nevi. J Am Acad Dermatol 2002; 46: 554- 556.
12. Alster TS. Inflammatory linear verrucous epidermal nevus: successful
treatment with the 585 nm flashlamp-pumped pulsed dye laser. J Am Acad
Dermatol 1994; 31: 513- 514.
13. Sidwell RU, Syed S,
Harper JI. Pulsed dye laser treatment for inflammatory linear verrucous
nevus. Br J Dermatol 2001; 144(6): 1267- 1269.
14.
Omura NE, Dover JS, Arndt KA, Kauvar AN. Treatment of reticular leg veins
with a 1064nm long-pulsed Nd: YAG laser. J Am Acad Dermatol 2003; 48: 76-
81.
15. Dover JS, Sadick NS, Goldman MP. The role of
lasers and light sources in the treatment of leg veins. Dermatol Surg 1999;
25: 328- 235.
16. Han TY, Lee JH, Lee CK, Ahn JY.
Long pulsed ND: YAG laser for treatment of warts: Report on a series of 369
cases. J Korean Med Sci 2009; 24: 889- 893.
17. Levy
J, Pons F, Agopian L, Besson R. Subjective and objective measurement methods
in cosmetic dermatology. Med Laser Appl 2004; 19: 223- 229.
18. Paradela S, Pozo J, Jorge B et al. Epidermal nevi treated by carbon
dioxide laser vaporization: A series of 25 patients. J Dermatolol Treatment.
2007; 18: 169- 174.
19. Welch ML, Smith KJ, Skelton
HG et al. Immunohistochemical features in inflammatory linear verrucous
epidermal nevi suggests a distinctive pattern of clonal dysregulation of
growth. J Am Acad Dermatol 1993; 29: 242- 248.
20.
Anderson RR, Parrish JA Selective photothermolysis: precise microsurgery by
selective absorption of pulsed radiation. Science 1983; 22: 524- 527.
21. Moller SJ, Poulsen T, Wulf HC. Investigative report. Epidermal thickness
at different body sites: relationship to age, gender, pigmentation, blood
content, skin type and smoking habits Acta Derm Venereol 2003; 83: 410- 413.
22. Boulnois JL. Photophysical processes in recent medical laser
developments: a review. Lasers Med Sci 1986; 1-17.
23. Groot D, Rao J, Johnston P, Nakatsui T. Algorithm for using a
long-pulsed Nd: YAG laser in the treatment of deep cutaneous vascular
lesions. Dermatol Surg 2003; 29: 35- 42.
24. Keller
R, JU´ Nior WB, Valente NYS, Rodrigues CJ. Nonablative 1,064-nm Nd:YAG Laser
for Treating Atrophic Facial Acne Scars: Histologic and Clinical Analysis.
Dermatol Surg 2007; 33(12): 1470- 1476.© 2010
Egyptian Dermatology Online Journal |