|
|
Abstract
Herpetic folliculitis is a very uncommon reported entity. It is also known as herpetic sycosis because it frequently affects the beard area. Atypical presentations (more common in immuno-suppressed patients) require histopathological confirmation of follicular involvement for diagnosis. To our knowledge we describe the first case in the literature affecting the buttocks. Polymerase chain reaction provides a more accurate diagnosis but is not widely available. Studies show suppressive therapy more effective than episodic one in genital herpes recurrences and this could be extrapolated to recurrent folliculitis of the buttocks. The later should be included in the differential diagnosis of recurrent pruritic lesions of the buttocks.
Case Report: Herpetic folliculitis has been seldom reported. Atypical presentations require histopathological confirmation of follicular involvement for diagnosis. It is also called herpetic sycosis because it frequently affects the beard area [1].To our knowledge we describe the first case in the literature affecting the buttocks. A 40-year-old woman with a 15 years history of systemic lupus erythematosus (SLE) treated with 1mg/kg/day of oral steroids consulted for having monthly recurrent episodes of pruritic vesicular lesions affecting the buttocks which spontaneously resolved in 4-5 days without scarring. She denied systemic symptoms or releasing causes. She sometimes used topical antibiotics without changing disease´s course. On examination she presented 2-4 mm follicular crusted lesions and erosions grouped over a reddish base on the buttocks
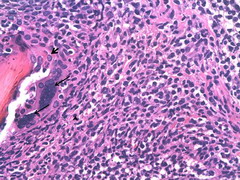
(Figure 1). Skin biopsy revealed herpetic cytopathic changes with ballooning, multinucleated epithelial cells and necrotic keratinocytes involving the infundibulum of the hair follicle with a lymphocytic infiltrate at the bottom (Figure 2 and 3). This led us to the diagnosis of herpetic folliculitis of the buttocks. The bilateral affectation, lack of severe pain and recurrence of episodes pointed to Herpes simplex virus (HSV) as the causal agent. She refused suppressive treatment and agreed with episodic acyclovir treatment: As normal renal function was confirmed doses of 200mg/ 4h, 5 times a day were prescribed at the first sign of prodromal symptoms of recurrence. After 5 months of follow up she reported shorter and lighter episodes and increment of free intervals.
 | Fig 1:
The buttocks of the patient showing follicular erosions and crusted
lesions grouped over an erythematous base in clusters. No vesicles
at this moment of could be appreciated. |
|
 | Fig
2: Skin biopsy stained with hematoxylin and eosin
showing dense and deep lymphocytic infiltrate around
follicles with necrosis of follicular keratinocytes,
ballooning cells and multinucleated epithelial cells (H&E X
4). |
|
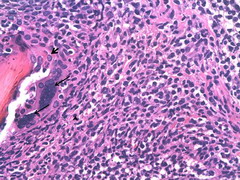 | Fig 1:
Higher magnification photomicrograph. Head arrow shows the dense
perifollicular infiltrate of lymphocytes; big arrows show the
multinucleated epithelial cells and small arrows the necrosis of
follicular keratinocytes (H&E X40). |
|
Herpetic folliculitis is an infrequent entity, with few cases reported. Atypical presentations require histopathological confirmation of follicular involvement for diagnosis. Typical vesicles are sometimes absent [1]. Diagnostic criteria are not well established and it is accepted that diagnosis can be made based on clinical and pathological morphology alone as in our patient [2]. Although not widely available, a more accurate diagnosis and differential detection of herpes virus types is obtained by Polymerase chain reaction (PCR).
Böer et al studied 21 cases showing that folliculitis involvement is more common in Varicella-zoster virus (VZV) than HSV infections [2,3]. Dense and deep infiltrates of lymphocytes especially around and within adnexal structures is a characteristic histopathological feature even in early stages. In HSV infections additional typical changes (ballooning, reticular alteration and acantholysis) in surface epidermis are present [2]. In contrast to the typical herpetic sycosis of the beard area in healthy males, we present affectation of the buttocks in an immune-suppressed woman. SLE patients have intrinsic and extrinsic incremented risk of infections. Esophagitis, interstitial pneumonitis or visual defects due to herpes virus have been described. Studies on the treatment of recurrent genital herpes, which could be extrapolated to recurrent herpetic folliculitis, concluded that although more expensive, a suppressive therapy is more effective than episodic one (longer time to first and between recurrences). Nevertheless it is important to take into account the patient´s preferences as in our case [4]. Other studies suggest similar effectiveness of 1 day treatment versus 2-5 conventional episodic therapies although more research is needed [5]. In conclusion, we present a case of herpetic folliculitis of the buttocks in an immune-suppressed patient with SLE. High rate of recurrence was present. Herpetic folliculitis should be included in the differential diagnosis of recurrent pruritic lesions of the buttocks. References
1. Herpetic Folliculitis. Shehab A. M. Al-Dhafiri. Journal of Cutaneous Medicine and Surgery.J Cutan Med Surg 2002; 19-22.
2. Herpes folliculitis: clinical, histopathological, and molecular
pathologic observations A. Böer, N. Herder, K. Winter and T. British Journal
of Dermatology 2006; 154: 743- 746
3. McSorley J, Shapiro L, Brownstein MH, et al. Herpes simplex and varicella-zoster: comparative histopathology of 77 cases. Int J Dermatol 1974; 13: 69- 75.
4. Romanowski B, Marina RB. Patients' preference of valacyclovir once-daily suppressive therapy versus twice-daily episodic therapy for recurrent genital herpes: a randomized study. Sex Transm Dis. 2003 Mar; 30(3): 226- 231
5. Tyring S, Berger T,Single-day therapy for recurrent genital herpes. Am J Clin Dermatol. 2006; 7(4): 209- 211.© 2010 Egyptian Dermatology Online Journal |