|
|
Abstract
Background
Dermoscopy is noninvasive optical surface microscopy, useful for
diagnostic purposes in a number of skin conditions including basal cell
carcinoma (BCC). Expert observers provide an accurate (sensitivity: 97%)
and reliable dermatoscopic diagnosis of BCC.
Objective
The aim of the study was to illustrate the effect of cryosurgery on
the dermoscopic findings in nodular basal cell carcinoma lesions.
Patients and methods
Ten patients complaining of nodular (n)BCC and treated by cryosurgery
were included.
Results and Conclusion
Disappearance of dermoscopic features was predictive of successful
treatment.
Dermoscopy is an effective method for follow-up of noninvasive
treatment modalities in cases of nBCC.
Introduction
Dermoscopy is noninvasive optical surface microscopy, useful for
diagnostic purposes in a number of skin conditions including basal cell
carcinoma (BCC) [1].
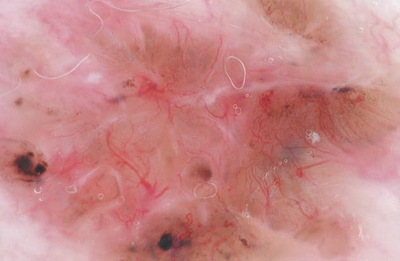
The classical dermoscopic findings for the diagnosis of BCC include
lack of a pigment network and the presence of at least one of the
following criteria: ulcerations, maple-leaf like structures, blue-grey
globules, blue-ovoid nests, arborizing vessels and spoke-wheel
structures [2]. (Fig 1)
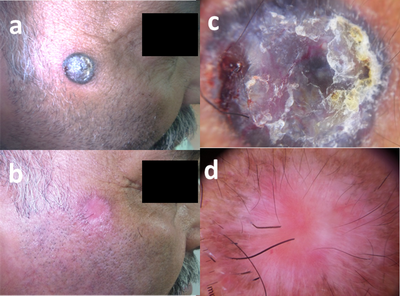
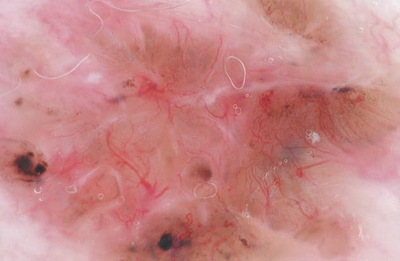 |
Fig 1: Pigmented basal cell carcinoma exhibiting arborizing
blood vessels, blue-gray globules and large blue-gray nests [2] |
|
Expert observers provide an accurate (sensitivity: 97%) and reliable
dermatoscopic diagnosis of BCC. Arborizing telangiectasia, leaf-like
areas, and large blue/gray ovoid nests represented reliable and robust
diagnostic parameters [3].
Treatment modalities for BCC include: standard excision, curettage
with or without electrodesiccation, Mohs micrographic surgery, radiation
therapy, cryosurgery, photodynamic therapy, laser ablation and medical
treatment in the form of 5-fluorouracil or imiquimod creams,
interferon-α-2bintralesional injections and oral vismodegib in addition
to various combined therapies. Nonablative therapeutic modalities are
licensed for the managementof superficial basal cell carcinoma (sBCC)
and lately have become very popular among dermatologists [4].
Recurrence rates for primary BCC vary with treatment modality. The
5-year recurrence rate for Cryotherapy may be as low as 7.5%, if lesions
are chosen judiciously [5]. Mallon and
Dawber studied the virtues of one versus two freeze-thaw cycles for
treatment of BCC and found that the double freeze-thaw cycle on the face
achieved 95.3% cure rate, whereas the single cycle had 79.4% cure rate [6].
As a result of the development of dermoscopy over the last three
decades, new targets have been added to its primary role of establishing
whether a lesion is suspicious for malignancy and necessitates biopsy or
follow-up [7-9].
Nowadays there is a tendency to use dermoscopy for pre-surgery
establishment of tumor borders and for monitoring the response of some
controllable cutaneous malignancies (such as lentigo maligna,
superficial basal cell carcinoma & Bowen's disease) to some topical
therapies [10-13].
Aim of the Work
The aim of work was to assess the success of cryosurgery in the
treatment of small nodular BCC lesions in addition to the periodic
follow-up of patients
Patients and Methods
Ten patients suffering from small nodular BCCs were enrolled in the
study
Exclusion criteria included:
- Lesions larger than 2 cms in diameter.
- Ischemic heart disease.
- Uncontrolled diabetes mellitus
- History of metastatic non-melanoma skin cancer.
- Lesions with high infiltration tendency (basi-squamous) and
infiltrative lesions.
- Any treatment or participation in another study in the last 30
days.
All BCCs were clinically and dermoscopically evaluated and digitally
documented using a hand held Dermlite DL3N dermoscope (3Gen, Inc., San
Juan Capistrano, California, USA.) and a 10x optical zoom Samsung S4
Zoom camera (Samsung Electronics Co., Ltd., Yeongtong-Gu Suwon-Shi,
South Korea) before starting treatment, before each session and during
every follow-up session for 1 year afterwards.
The treatment plan was to perform a weekly session of two freeze-thaw
cycles of liquid nitrogen Cryospray using the Brymill Cry-AC (Brymill
Cryogenics Systems, Ellington, Connecticut, USA) on the target area
(tumor and a perilesional margin of 5mm), each lasting for 20-30
seconds.
Results
Ten patients suffering from nBCC participated in the study.
Prevalence of dermoscopic findings in these patients was as follows:
microulcerations (80%), arborizing blood vessels and blue grey globules
(70% each), maple leaf like structures, blue grey ovoid nests (30%) and
peppering (20%).
There was gradual disappearance of the dermoscopic findings during
the treatment sessions which were continued till all dermoscopic
findings disappeared and replaced by rosy whitish diffuse areas with or
without small dotted blood vessels.
No signs of recurrence were seen in all patients during the one year
follow-up period indicated by the presence of diffuse white scar tissue
and maintained absence of dermoscopic structures seen at the initial
visit (fig 2, 3, 4).
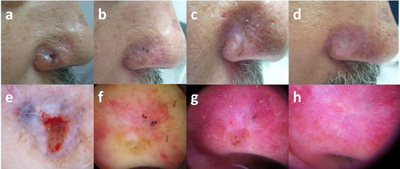 |
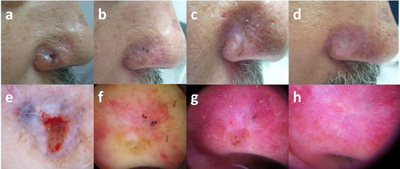
Fig 2: 52-year-old male patient, (a) initial visit,
(b) after 2 sessions, (c) after 4 sessions, (d)
after 6 sessions, (e-h) corresponding dermoscopic images
(20x, contact, polarized) showing gradual disappearance of the
initial ulceration, white structureless areas, blue grey globules
and nests till complete cure (rosy white diffuse area). |
|
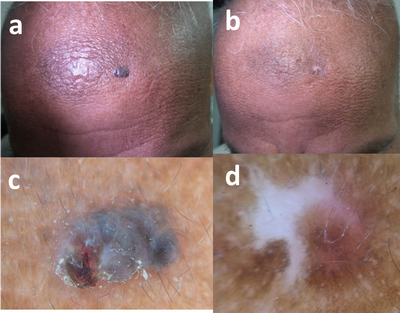
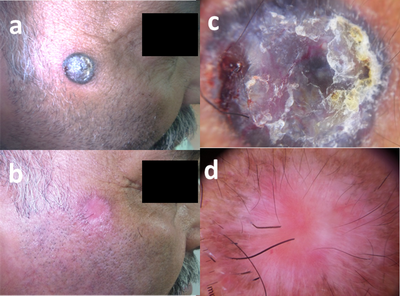
 | Fig 3: 63-year-old male patient, (a) initial visit,
(b) 1 year after last session, (c) dermoscopy (30x, contact,
polarized) in initial session shows diffuse blue grey ovoid nests and
microulceration, (d) after 1 year follow up, only white scar
tissue is present with progressive repigmentation from the periphery. |
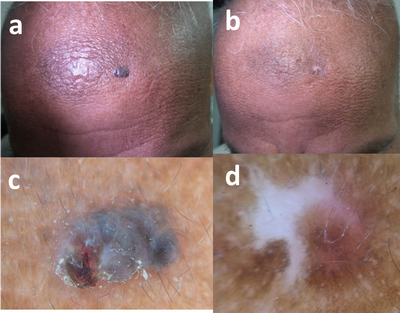
|
 | Fig
4 : 49-year-old male patient, (a) initial visit,
(b) after 5 sessions, (c) dermoscopy (15x, contact,
polarized) in initial session shows diffuse blur grey ovoid nests,
arborizing blood vessels and microulceration, (d) disappearance
of the initial findings and replaced by rosy white diffuse area. |
|
Discussion
Dermoscopy has become an integrative part of the clinical examination
of skin tumors. This is because it significantly improves the early
diagnosis of melanoma and non-melanoma skin cancer (NMSC) including
basal cell carcinoma and keratinocyte skin cancer compared with the
unaided eye. Besides its value in the noninvasive diagnosis of skin
cancer, dermoscopy has also gained increased interest in the management
of NMSC. Dermoscopy has been used in the preoperative evaluation of
tumor margins, monitoring of the outcomes of topical treatments and
post-treatment follow-up therapies [14].
Apalla and coworkers in 2014 studied the applicability of dermoscopy
in the evaluation of the outcome and monitoring of superficial basal
cell carcinoma (sBCC) after nonablative therapies. They suggested that
certain dermoscopic criteria, namely pigmented structures, ulceration
and arborizing vessels, predict the presence of residual disease
[residualdisease-associateddermoscopiccriteria(RDADC)] and they aimed to
assess this hypothesis by biopsying lesions exhibiting RDADC 3 months
after treatment and in the case of histopathological confirmation were
excised, however lesions characterized by white/red structureless areas,
superficial fine telangiectasias, or lacking any dermoscopic criterion,
were monitored for 12 months. At the 3-month evaluation, one or more of
the RDADC were detected in 25/98 (25·5%) sBCCs, in which histology
confirmed tumor persistence. In 45 (61·6%) of the 73 remaining lesions,
dermoscopy showed white/red structureless areas and/or superficial fine
telangiectasias. Twenty-eight lacked any dermoscopic criterion of sBCC.
The two latter groups entered follow-up. In total, disease recurred in
13 (17·8%) of the 73 lesions. Based on that they concluded that RDADC
accurately predict residual disease. Absence of dermoscopic criteria of
sBCC safely predicts complete histopathological clearance. Detection of
white/red structureless areas and/or superficial fine telangiectasias
warrants close monitoring to recognize early recurrence. [15].
In our study, we used an efficient topical destructive therapy for
small nBCCs, which is liquid nitrogen spray cryosurgery (5 year cure
rate = 92%), and we didn't stop sessions unless complete disappearance
of all dermoscopic structures was evident and no recurrence was seen
neither clinically nor dermoscopically for a one year follow-up,
indicating that absence of dermoscopic structures can be really
dependable in follow-up of non-invasive modalities of treatment for BCC.
Conclusion
Cryosurgery is an effective method in the treatment of basal cell
carcinoma patients and dermoscopy is also an effective and dependable
tool for follow-up of non-invasive treatment modalities generally and
cryosurgery specifically in cases of nBCC.
References
1. Gérald E, Pierard, Piérard-Franchimont Claudine,
Hermanns Jean-François, Caucanas Marie, and Delvenne Philippe. "Analytic
dermoscopy of superficial basal cell carcinoma." Journal of Case Reports
in Medicine 2013 (2013).
2. Malvehy J, Puig S, Braun, RP, Marghoob, AA, Kopf AW:
Handbook of Dermoscopy, Taylor & Francis, London, 2006. pp. 86.
3. Altamura D, Menzies S, Argenziano G, Zalaudek I,
Soyer P, Sera F, Avramidis M, DeAmbrosis K, Fargnoli M, Peris K.
Dermatoscopy of basal cell carcinoma: Morphologic variability of global
and local features and accuracy of diagnosis, January 2010,Volume 62,
Issue 1, p. 67-75.
4. Roozeboom MH, Arits AH, Nelemans PJ, Kelleners-Smeets
NW. Overall treatment success after treatment of primary superficial
basal cell carcinoma: a systematic review and meta-analysis of
randomized and nonrandomized trials. Br J Dermatol 2012; 167:733-56.
5. Kuflik EG, Gage AA. The five-year cure rate achieved
by cryosurgery for skin cancer. J Am Acad Dermatol 1991; 24:1002-1004.
6. Mallon E, Dawber R. Cryosurgery in the treatment of
basal cell carcinoma. Assessment of one and two freeze-thaw cycle
schedules. Dermatol Surg1996; 22:854-858.
7. Puig S, Argenziano G, Zalaudek I, Ferrara G, Palou J,
et al. (2007) Melanomas that failed dermoscopic detection: a combined
clinicodermoscopic approach for not missing melanoma. DermatolSurg 33:
1262-1273.
8. Benvenuto-Andrade C, Dusza SW, Agero AL, Scope A,
Rajadhyaksha M, et al. (2007) Differences between polarized light
dermoscopy and immersion contact dermoscopy for the evaluation of skin
lesions. Arch Dermatol 143: 329-338.
9. Terushkin V, Wang SQ (2009) Mohs surgery for basal
cell carcinoma assisted by dermoscopy: report of two cases. DermatolSurg
35: 2031-2035.
10. Caresana G, Giardini R (2010) Dermoscopy-guided
surgery in basal cell carcinoma. J EurAcadDermatolVenereol 24:
1395-1399.
11. Mun JH, Kim SH, Jung DS, Ko HC, Kwon KS, et al.
(2010) Dermoscopic features of Bowen's disease in Asians. J
EurAcadDermatolVenereol 24: 805- 810.
12. Fargnoli MC, Kostaki D, Piccioni A, Micantonio T,
Peris K (2012) Dermoscopy in the diagnosis and management of
non-melanoma skin cancers. Eur J Dermatol 22: 456-463.
13. Carli P, de Giorgi V, Palli D, Giannotti V,
Giannotti B (2000) Preoperative assessment of melanoma thickness by ABCD
score of dermatoscopy. J Am AcadDermatol 43: 459-466.
14. Lallas A, Argenziano G, Zendri E, Moscarella E,
Longo C, Grenzi L, Pellacani G, Zalaudek I. Update on non-melanoma skin
cancer and the value of dermoscopy in its diagnosis and treatment
monitoring.Expert Rev Anticancer Ther. 2013 May;13(5):541-58.
15. Apalla Z, Lallas A, Tzellos T, Sidiropoulos T,
Lefaki I, Trakatelli M, Sotiriou E, Lazaridou E, Evangelou G, Patsatsi
A, Kyrgidis A, Stratigos A, Zalaudek I, Argenziano G, Ioannides D.
Applicability of dermoscopy for evaluation of patients' response to
nonablative therapies for the treatment of superficial basal cell
carcinoma. Br J Dermatol. 2014 Apr;170(4):809-15.
© 2015 Egyptian Dermatology Online Journal
|